Key takeaways:
- Individuals with HIV had a decrease chance of receiving therapy for most cancers in the event that they lived in areas with low revenue and low instructional attainment.
- Disparities endured regardless of insurance coverage sort and therapy middle.
Greater than 15% of people dwelling with HIV and most cancers haven’t acquired beneficial first-line most cancers remedy, in keeping with outcomes of a retrospective evaluation.
Amongst sufferers with HIV and most cancers, those that lived within the lowest quartiles for revenue or instructional attainment had considerably decrease odds of getting most cancers therapy in contrast with these within the high quartiles.

Information derived from Islam JY, et al. Most cancers. 2025;doi:10.1002/cncr.35881.

Jessica Y. Islam
“Individuals dwelling with HIV, so long as their HIV is well-controlled, ought to obtain the identical precise [cancer] care as somebody who is just not dwelling with HIV,” Jessica Y. Islam, PhD, MPH, assistant professor of most cancers epidemiology at Moffitt Most cancers Heart, advised Healio.
Inequity has ‘endured over time’
Islam and colleagues revealed a report in Journal of Scientific Oncology in 2024 that discovered folks with HIV had considerably increased odds of not getting most cancers therapy for a number of malignancy varieties in contrast with those that didn’t have HIV between 2001 and 2019.
“This inequity by HIV standing has endured over time,” Islam mentioned.
Different research have proven people with HIV and most cancers have worse cancer-specific survival than these with out HIV, in keeping with examine background.
Sufferers with HIV not getting beneficial most cancers screening and therapy has factored into these knowledge.
“What’s it about folks dwelling with HIV [not getting treatment]?” Islam requested. “Is it the biology, or are there social elements which are taking part in into this? The social piece is necessary due to the historic distribution of HIV an infection inside the US. We all know that throughout the U.S., the HIV epidemic persists amongst marginalized populations reminiscent of Black and Hispanic adults, males who’ve intercourse with males, and different demographic teams which are disenfranchised from the well being care system.
“These obstacles inside folks dwelling with HIV exist already,” she continued. “Once we come into the most cancers house, how does that play out inside this inhabitants?”
Islam and colleagues used the Nationwide Most cancers Database, a registry sponsored by the American Faculty of Surgeons and American Most cancers Society that features greater than 70% of U.S. most cancers instances, to research.
They included 31,549 people identified with HIV and most cancers (43.2% aged 60 years and older; 50.5% white; 37.5% Black; 68.4% males) of their examine.
The database included two socioeconomic elements based mostly on zip code — proportion of adults who didn’t have a highschool diploma and median family revenue.
Receipt of first-line most cancers therapy based mostly on these measures served as the first endpoint.
Poverty impacts most cancers therapy
In all, 16.5% of the examine inhabitants didn’t obtain first-line therapy for his or her most cancers.
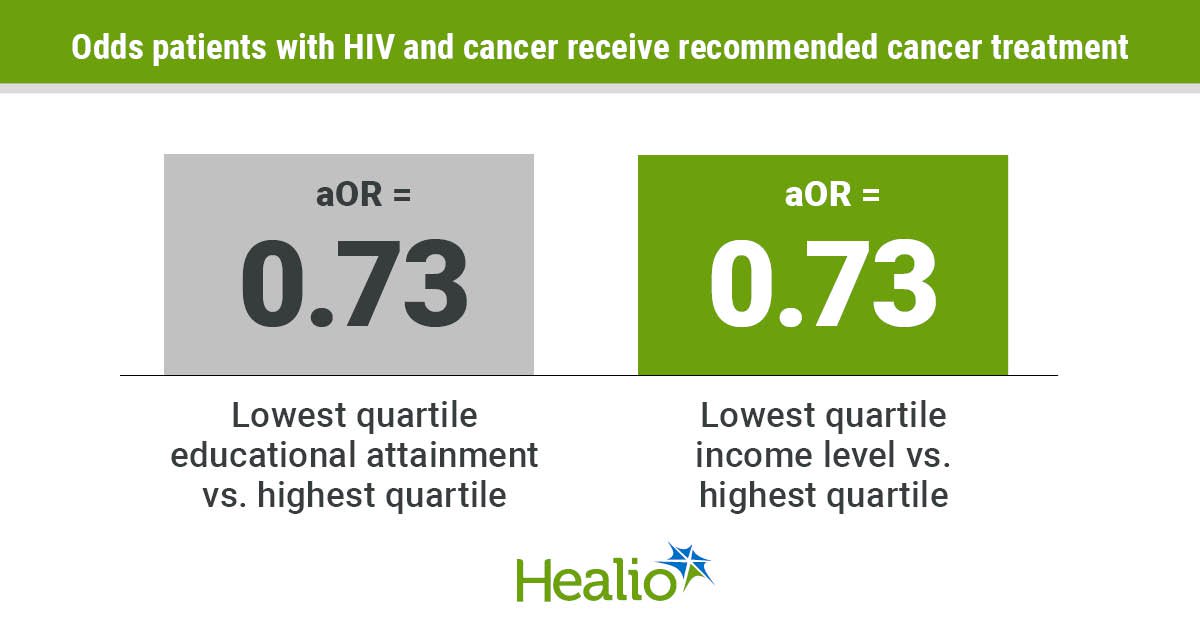
Sufferers who lived within the lowest quartile of instructional attainment had considerably decrease odds of receiving most cancers therapy in contrast with the best quartile (adjusted OR = 0.73; 95% CI, 0.66-0.82). These within the second lowest quartile additionally had considerably decrease odds than the best quartile (aOR = 0.85; 95% CI, 0.77-0.95).
Moreover, sufferers who lived within the lowest quartile of revenue had considerably decrease odds of getting beneficial most cancers remedy in contrast with the highest quartile (aOR = 0.73; 95% CI, 0.65-0.81). These within the second lowest quartile additionally had considerably decrease odds in contrast with the best quartile (aOR = 0.83; 95% CI, 0.74-0.94).
“My preliminary speculation going into this challenge was that people who find themselves dwelling in decrease useful resource settings can be much less more likely to obtain therapy. That didn’t shock me,” Islam mentioned. “What did shock me was this affiliation has endured. I did anticipate the affiliation to type of dwindle over time, however we see that it’s nonetheless one thing occurring in current day.”
Disparities endured regardless of insurance coverage sort, most cancers therapy facility and distance to care.
“Essentially the most placing one was stratification by most cancers therapy facility sort, the place we noticed that for many who acquired care at a tutorial analysis program — which must be the best high quality of care — poverty nonetheless performed a task inside their odds of receiving most cancers therapy,” Islam mentioned. “That was true for each lowest instructional attainment and lowest median revenue.”
Researchers acknowledged examine limitations, together with being restricted to zip-code degree knowledge.
Islam emphasised the necessity for analysis based mostly on extra “granular” knowledge.
“For instance, at a tutorial analysis most cancers therapy facility, what are the interactions with totally different well being care suppliers, or throughout the system that could be contributing to this disparity that we will intervene on?” she mentioned.
‘Preserve them engaged’
Islam and colleagues have carried out qualitative interviews with sufferers to debate their experiences receiving care.
“These are people who could have been dwelling with HIV for over 2 a long time,” Islam mentioned. “Somebody who’s dwelling with a power illness, particularly HIV, and so they’ve survived this lengthy, they’ll hear a giant analysis like most cancers and assume, ‘I’ve survived this lengthy, and I need to stay the remainder of my life comfortably with none symptomology related to getting such a tough therapy.’ Typically they refuse therapy.”
Different people have reported emotions of discrimination.
“That won’t have occurred particularly on the most cancers hospital, however simply bringing in experiences from their HIV care over time, it does influence how they understand their most cancers therapy expertise,” Islam mentioned.
These previous experiences additionally could cease sufferers from disclosing their HIV historical past.
Lindsay N. Fuzzell, PhD, utilized analysis scientist at Moffitt, and colleagues revealed a report in JNCI Most cancers Spectrum in 2021 that discovered solely 36.1% of sufferers with HIV and most cancers at Moffitt between 2009 and 2019 disclosed their HIV standing.
“A policy-level change to enhance this subject could possibly be instituting a requirement that we blanket take a look at for sufferers with HIV or simply different power immune-suppressive circumstances,” Islam mentioned.
Figuring out HIV standing won’t assure therapy, although. Islam emphasised the significance of interventions to extend the variety of sufferers getting the care they want.
“Those that reside with HIV could produce other health-related social wants that will not be arising throughout their conversations,” Islam mentioned. “Suppliers ought to at all times contemplate referring them to social companies or making certain they know that’s an choice to hold them engaged with their most cancers therapy to completion.”
References:
For extra data:
Jessica Y. Islam, PhD, MPH, could be reached at jessica.islam@moffitt.org.