Key takeaways:
- Predictors of revision endoscopic sinus surgical procedure at 1 yr and three years after preliminary surgical procedure included baseline antibiotic use and age.
- Baseline oral corticosteroid use and bronchial asthma have been solely predictors for 1 yr.
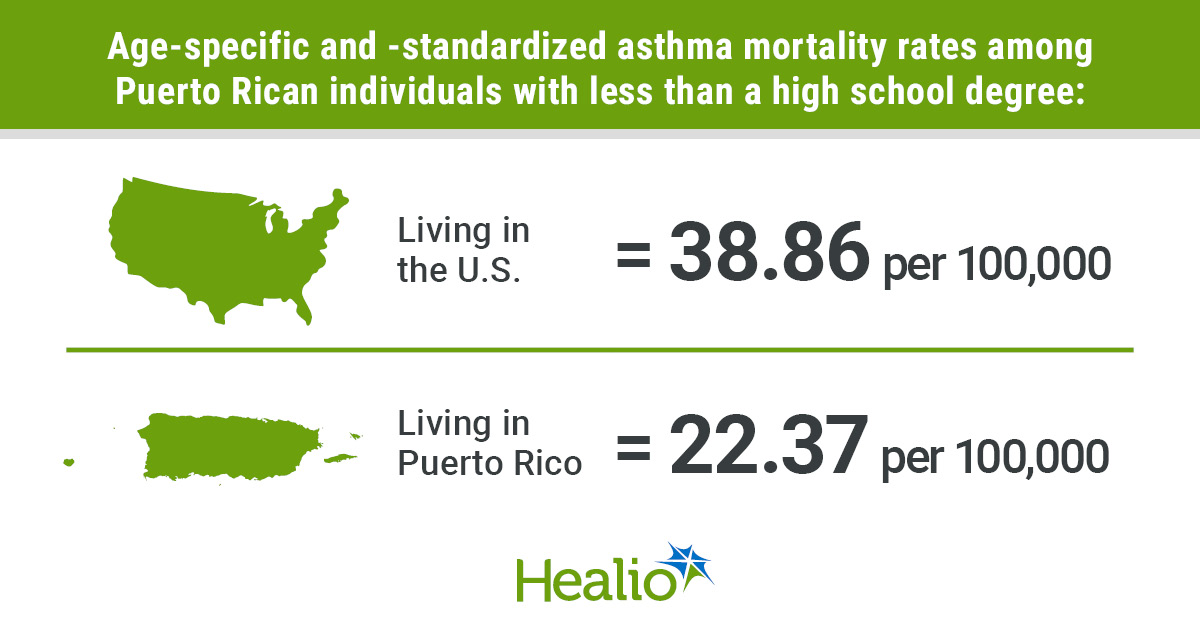
In sufferers with power rhinosinusitis with nasal polyps, components together with baseline antibiotic use and bronchial asthma impacted the chances for revision endoscopic sinus surgical procedure, in accordance with knowledge printed in Scientific and Translational Allergy.
“Affected person’s bronchial asthma standing and the variety of antibiotic and oral corticosteroid programs must be thought of when considering surgical procedure,” Sanna Toppila-Salmi, MD, PhD, professor of otorhinolaryngology on the College of Jap Finland, advised Healio.

On this population-based examine, Toppila-Salmi and colleagues evaluated 3,506 adults (median age, 55 years; 72% males) with CRSwNP who underwent endoscopic sinus surgical procedure (ESS) to uncover what components enhance the probability for revision surgical procedure at two time factors after the preliminary surgical procedure: 1 yr and three years.
The follow-up interval spanned from January 2012 to December 2019 (median, 4.3 years), and on this time, 559 (15.9%) adults underwent one revision surgical procedure and 153 (4.4%) underwent two or extra revision surgical procedures (median time to revision, 425 days).
Toppila-Salmi advised Healio the youthful median age of sufferers with two or extra revision surgical procedures vs. sufferers with no revision surgical procedure was surprising (48 vs. 56 years; P < .001).
When assessing oral corticosteroid use, researchers reported that the proportion of sufferers with baseline use was bigger amongst these with two or extra vs. no revision surgical procedures (63% vs. 49%; P < .001). Additional, these with a number of revision surgical procedures had a median day by day dose of three.29 mg, which was considerably higher than the 1.64 mg dose discovered for these with out revision surgical procedure (P < .001).
In accordance with the examine, a higher proportion of sufferers with revision surgical procedure underwent this surgical procedure inside 3 years vs. 1 yr from the preliminary surgical procedure (20.9% [n = 421] vs. 10.2% [n = 322]).
At each follow-up factors, researchers discovered that the kind of ESS surgical procedure initially given impacted the chances for revision surgical procedure, with a considerably higher probability for this final result with preliminary in depth vs. restricted surgical procedure (1 yr, adjusted OR = 3.33; 95% CI, 1.19-8.09; 3 years, aOR = 14.13; 95% CI, 3.41-95.64).
“The extra in depth the preliminary surgical procedure, the upper the chance of revision surgical procedure” was an surprising discovering, Toppila-Salmi advised Healio.
Researchers additionally noticed a big elevated probability for revision ESS inside 1 yr and three years of preliminary surgical procedure with vs. with out baseline antibiotic use (1 yr, aOR = 1.58; 95% CI, 1.23-2.03; 3 years, aOR = 1.61; 95% CI, 1.27-2.04).
Heightened odds for revision surgical procedure have been moreover discovered at each time factors for sufferers with vs. with out bronchial asthma at baseline (1 yr, aOR = 1.4; 95% CI, 1-1.92; 3 years, aOR = 1.58; 95% CI, 1.17-2.12); nevertheless, the examine reported that the 1-year discovering was a “marginal affiliation.”
Components linked to a decreased probability for revision surgical procedure included baseline oral corticosteroid use (1 yr, aOR = 0.69; 95% CI, 0.53-0.89) and better age at preliminary surgical procedure per 10 years (1 yr, aOR = 0.93; 95% CI, 0.86-1 [“marginal association”]; 3 years, aOR = 0.82; 95% CI, 0.76-0.88), in accordance with the examine.
At each 1 yr and three years, baseline intranasal corticosteroid common use was not considerably linked to the chances for revision surgical procedure, and this was additionally true for baseline Charlson Comorbidity Index rating.
Primarily based on Shapley values, researchers noticed 4 “key predictors” of revision ESS on the 1-year mark: baseline antibiotic use, baseline oral corticosteroid use, age and baseline bronchial asthma. Age and baseline antibiotic use additionally emerged as “vital predictors” on the 3-year mark.
The ultimate a part of this examine evaluated how 4 totally different combos of antibiotic use and bronchial asthma change the anticipated chance of revision ESS in a person aged 55 years (common affected person on this inhabitants) 3 years after preliminary surgical procedure.
The mix with the best predicted chance was antibiotic use plus bronchial asthma (23%), adopted by no antibiotics plus bronchial asthma (16%), antibiotics plus no bronchial asthma (16%) and no antibiotics plus no bronchial asthma (11%).
Wanting forward, Toppila-Salmi advised Healio future research could evaluate “the impact of operative and biologic remedy.”
Reference:
For extra data:
Sanna Toppila-Salmi, MD, PhD, will be reached at sanna.salmi@helsinki.fi.