August 08, 2025
10 min learn
A 56-year-old lady with a historical past of relapsed/refractory IgG kappa a number of myeloma offered with a 3-day historical past of proper eye redness, ache, photophobia and profound visible decline.
She reported frequent in a single day put on of day by day disposable smooth contact lenses.

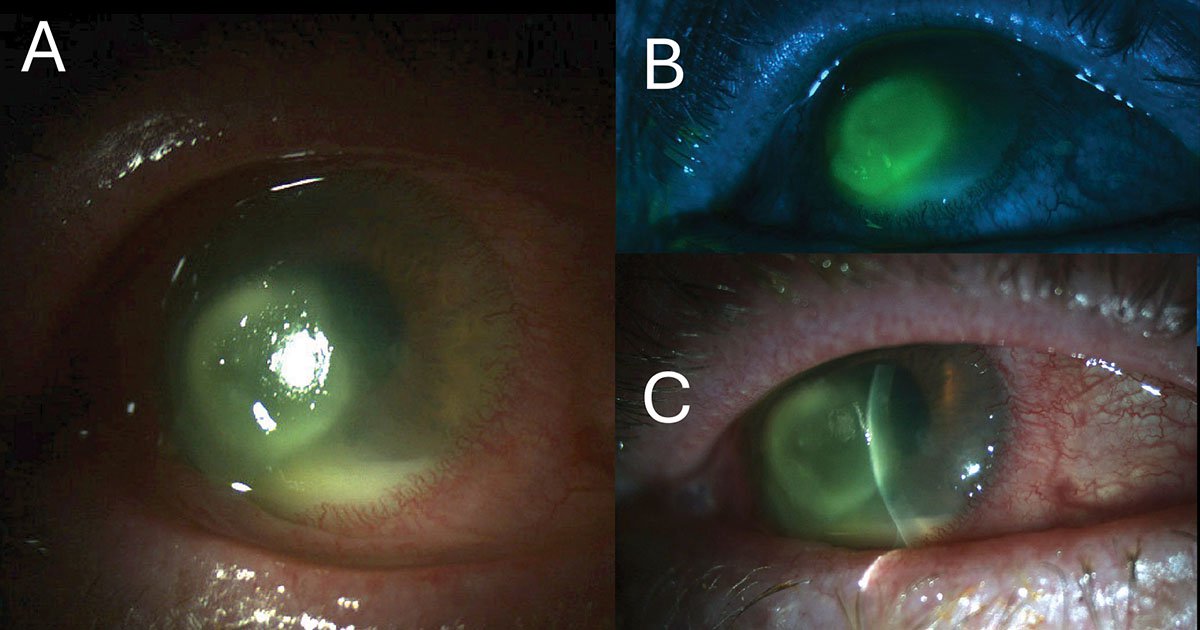
Supply: Hamid Alemi, MD, MPH, and Sarkis H. Soukiasian, MD
Her signs started after an eyebrow waxing session throughout which she rubbed her proper eye whereas sporting her lenses. The next day, she famous worsening irritation and changed her contact lenses for consolation. Over the following 2 days, there was progressive redness, discomfort and blurred imaginative and prescient, prompting her to put on an eye fixed patch. She sought medical analysis on the third day resulting from additional ache and visible deterioration.
She was a recurring smooth contact lens wearer with poor hygiene practices, together with in a single day put on. She denied any historical past of ocular trauma with vegetative materials, freshwater publicity or faucet water use for lens care. There was no historical past of herpes simplex or zoster keratitis, nor prior use of topical corticosteroids, topical anesthetics, NSAIDs or homeopathic eye drops. She additionally denied leisure drug use, together with cocaine. No ocular medicines had been used previous to presentation.
Her ocular historical past included myopia and proper eye blepharoplasty. Her systemic medical historical past was important for relapsed/refractory a number of myeloma identified in 2023, initially handled with daratumumab, lenalidomide, bortezomib and dexamethasone. At presentation, she was receiving lenalidomide 10 mg day by day and dexamethasone 4 mg (days 1 to 21 of a 28-day cycle); her most up-to-date daratumumab infusion had been 2 weeks prior. Extra medicines included valacyclovir 1,000 mg day by day for viral prophylaxis and aspirin 81 mg day by day. Her analgesic routine consisted of extended-release morphine 30 mg twice day by day, gabapentin 300 mg two to a few instances day by day, acetaminophen 500 mg thrice day by day, naproxen 220 mg twice day by day (in taper) and oxycodone 10 mg as wanted.
Examination
On presentation, uncorrected visible acuity was mild notion in the suitable eye and 20/30 within the left, enhancing to twenty/20 with pinhole. IOP was 13 mm Hg in the suitable eye and 15 mm Hg within the left. Pupils have been equal and reactive with out a relative afferent pupillary defect. Extraocular actions have been full and orthotropic bilaterally. Slit lamp images of the suitable eye are proven in Determine 1. Exterior examination revealed higher eyelid edema and erythema on the suitable with out proof of malposition, vesicular rash or preauricular lymphadenopathy. Lashes have been current with out particles or collarettes. The conjunctiva demonstrated 3 to 4+ injection with marked inferior chemosis. Corneal sensation was diminished within the affected eye with a 4.7 mm × 7 mm central epithelial defect extending inferotemporally, overlying a dense 4.6-mm ring infiltrate with irregular margins and surrounding stromal haze. A big infiltrate was famous temporally on the perilimbal space, related to overlying mucopurulent materials. There was minimal stromal thinning with out corneal perforation or descemetocele. The anterior chamber was deep, with 4+ cells, intense flare and 1.5-mm inferior hypopyon. The iris was small and flat with out nodules, neovascularization, heterochromia or notable synechiae. The lens couldn’t be clearly visualized resulting from stromal opacity.
The left eye examination was inside regular limits.
Imaging
Ultrasonography of the suitable eye was obtained on the day of presentation resulting from poor visualization of the posterior phase, revealing no indicators of vitritis, endophthalmitis or scleritis (Determine 2).

What’s your prognosis?
See reply beneath.
Contact lens wearer
The preliminary presentation of this affected person — a contact lens wearer with subacute onset of ocular ache, photophobia, redness and a visual hypopyon — prompted fast concern for microbial keratitis.


Slit lamp examination demonstrated a big central epithelial defect with underlying stromal infiltrate, important anterior chamber irritation, and no indicators of scleritis or posterior phase involvement. Given the medical findings and a historical past of power in a single day contact lens put on, bacterial keratitis, notably Pseudomonas aeruginosa, was thought of the most certainly prognosis, given its well-established affiliation with contact lens-related ulcers and its potential for fast development to corneal melting and imaginative and prescient loss if left untreated. Herpetic keratitis was additionally included within the differential, owing to the affected person’s immunosuppressed standing. Fungal keratitis remained a diagnostic consideration, though the historical past lacked traditional threat components reminiscent of trauma with vegetative materials or current publicity to agricultural environments. Acanthamoeba keratitis was additionally thought of; nonetheless, the absence of key epidemiologic threat components, together with publicity to freshwater, swimming in lenses or noncompliance with disinfection protocols, made this prognosis much less doubtless. The fast growth of keratitis was additionally not per subacute presentation of signs of fungal and Acanthamoeba keratitis. Topical anesthetic toxicity was deemed unbelievable primarily based on each historical past and medical presentation: The affected person denied any use of topical anesthetics, had no behavioral threat components reminiscent of medicine entry or substance use, and retained intact corneal sensation.
Workup and administration
We pursued a scientific and empiric preliminary method for infectious corneal ulcer. Corneal scrapings have been obtained for Gram staining, cardio and anaerobic bacterial tradition, fungal tradition, and PCR testing for fungal species and viruses together with herpes simplex and varicella-zoster virus. Given the massive central location of the infiltrate and related visible compromise, empiric broad-spectrum antimicrobial remedy was initiated. Hourly fortified tobramycin (15 mg/mL) and moxifloxacin 0.5% have been chosen to offer synergistic protection towards gram-negative and gram-positive organisms, together with Pseudomonas aeruginosa, a frequent and virulent pathogen in touch lens-associated keratitis. Within the absence of prior MRSA colonization and given the community-acquired nature of the an infection, empiric protection for MRSA was deferred.
Though dendritiform epithelial lesions have been absent, the affected person’s immunocompromised standing raised suspicion for herpetic keratitis. Certainly, herpetic keratitis in immunocompromised hosts can current atypically, missing the traditional dendritic epithelial lesions seen in immunocompetent people. Oral valacyclovir was escalated from prophylactic to therapeutic dose (1,000 mg thrice day by day) to empirically cowl herpes simplex and varicella-zoster virus-associated keratouveitis. Adjunctive remedy with oral doxycycline (100 mg day by day) and vitamin C have been initiated to scale back stromal collagenolysis and collagen synthesis. Cyclopentolate was prescribed for cycloplegia and prevention of posterior synechiae. With approval from the medical oncology crew, lenalidomide and dexamethasone have been withheld resulting from concern for immunosuppression-related an infection. The affected person was monitored intently. By day 3, early indicators of epithelial therapeutic have been noticed, with a discount within the dimension of the epithelial defect and hypopyon, accompanied by delicate enchancment in visible acuity. In response, topical fortified tobramycin and moxifloxacin have been tapered progressively, whereas valacyclovir was continued.
Nonetheless, from day 3 to day 7, there was no important enchancment in imaginative and prescient, which was depend fingers at face, with delayed medical decision, elevating concern for pathogens not coated by the preliminary antimicrobial routine. Anterior phase OCT (AS-OCT) carried out on day 7 demonstrated anterior to mid-stromal haze with refined irregularities of Descemet’s membrane and posterior stromal undulations, which recommend deep or full-thickness corneal involvement, not particular to any etiology (Determine 3). Due to this fact, in vivo confocal microscopy (IVCM) was executed and confirmed filamentous, hyperreflective, branching constructions suspicious for filamentous fungi with a diffuse stromal hyperreflectivity indicative of fibrosis and irritation (Determine 4). Cultures have been repeated by corneal scraping of the infiltrates, and at this stage, 7 days after the preliminary encounter, empiric antifungal remedy with topical amphotericin B 0.15% was initiated hourly as a result of excessive suspicion on imaging. Natamycin, the first-line remedy for filamentous fungal keratitis, was unavailable resulting from price and restricted entry. Amphotericin was chosen for its accessibility and broad-spectrum antifungal exercise. Inside 4 days of initiating amphotericin, there was marked visible enchancment and dramatic regression of the corneal epithelial infiltrate and hypopyon. Tobramycin and valacyclovir have been progressively tapered; moxifloxacin was maintained 4 instances day by day to stop secondary bacterial an infection. After 4 weeks of therapy with amphotericin, visible acuity improved to twenty/70, and slit lamp examination demonstrated decision of the epithelial defect, anterior stromal haze and scarring, with solely a low-grade anterior chamber response; due to this fact, amphotericin was tapered over 4 weeks. All topical antibiotics have been discontinued by 2 months. Regardless of persistently damaging cultures, the medical response to amphotericin, supported by AS-OCT and confocal findings, strongly favored a prognosis of fungal keratitis. The timeline of workup and administration is depicted in Determine 5.


Dialogue
Tradition-negative microbial keratitis poses substantial diagnostic and therapeutic challenges. Whereas microbiologic tradition stays the diagnostic gold customary, its sensitivity is diminished, notably in instances with prior antimicrobial publicity or deep stromal involvement. In a retrospective evaluate of 933 instances, Venugopal and colleagues discovered that 66.7% have been each smear- and culture-negative. Amongst these reevaluated, 50% yielded optimistic outcomes on repeat microbiologic testing, with fungal organisms accounting for greater than 60% of isolates.

Within the mentioned case, bacterial and fungal cultures and PCR confirmed no progress. Lack of response to broad-spectrum antibiotic remedy raised suspicion for different infectious keratitis, together with fungal etiology. AS-OCT didn’t present findings suggestive of fungal keratitis, described within the literature as stromal cystic areas or endothelial plaques with overlying junctional hole with posterior stroma (Jin et al.; Soliman et al.). IVCM demonstrated skinny, hyperreflective, branching filaments inside the anterior stroma, suggestive of filamentous fungi or Pythium insidiosum. Whereas these organisms have overlapping morphologic options, therapy differs considerably: Pythium insidiosum, a waterborne oomycete that mimics fungal an infection, requires therapy with brokers reminiscent of linezolid or azithromycin or surgical intervention. In distinction, filamentous fungal keratitis sometimes responds to antifungal brokers reminiscent of amphotericin B or natamycin. On this case, the fast medical response to amphotericin B additional supported a fungal relatively than Pythium etiology (Chidambaram et al.).
IVCM is very worthwhile in culture-negative instances, with reported sensitivity and specificity of 89% and 78%, respectively, for fungal keratitis (Vaddavalli et al.). These imaging findings facilitated the well timed initiation of empiric antifungal remedy in our case.
Presently, no common consensus exists on when to provoke empiric antifungal therapy in suspected microbial keratitis. Nonetheless, professional opinion and medical knowledge assist early empiric protection within the setting of threat components reminiscent of immunosuppression, atypical ulcer morphology or poor antibiotic response (Amescua et al.; Prajna et al.). If cultures are damaging or therapy is ineffective, repeating cultures by means of corneal scraping or performing a corneal biopsy could also be thought of. An antimicrobial vacation earlier than re-culture can improve diagnostic yield however should be balanced towards the chance for medical deterioration.
Longitudinal IVCM imaging presents not solely diagnostic utility but additionally therapeutic monitoring. Repeat IVCM can assess for persistent microbial constructions and information therapy period, particularly when preliminary findings are equivocal or tradition is damaging (Nielsen et al.). Background irritation, scarring and stromal edema might obscure or mimic fungal options on imaging. Thus, early and serial imaging, mixed with medical course and response to therapy, helps set up prognosis of fungal keratitis. Nonetheless, the utility of IVCM is very operator dependent. Diagnostic accuracy depends not solely on technical execution but additionally on the experience of the examiner, the picture selector and the picture interpreter (Bakken et al.). Importantly, there’s additionally an image-quality depth limitation of IVCM when imaging keratitis involving deep tissue, corneal opacities and invasion to the anterior phase — thus, the significance of excessive suspicion, early and repeat imaging on this situation.
On this case, antifungal remedy resulted in fast visible enchancment, from hand movement to twenty/70, and backbone of epithelial defect and hypopyon inside 1 week. Ongoing IVCM was deliberate to watch therapy response and information tapering. Given the affected person’s immunosuppressed state and use of brokers reminiscent of lenalidomide and daratumumab, each of which can impair epithelial therapeutic, shut follow-up is important.
Conclusion
The analysis of corneal ulcers stays difficult resulting from overlapping threat components and medical options throughout completely different etiologies. Whereas affected person historical past and examination information the preliminary evaluation, definitive prognosis typically depends on microbiologic tradition following corneal scraping. Though tradition is the gold customary, its sensitivity will be restricted, notably in deep stromal infections or instances reminiscent of fungal keratitis, by which progress is gradual and yields are sometimes low. Invasive procedures reminiscent of corneal biopsy could also be obligatory in choose instances however carry dangers for tissue injury. IVCM presents a worthwhile noninvasive adjunct by enabling visualization of fungal constructions, together with hyphae and spores, and may assist in each prognosis and monitoring therapy response. Common follow-up and early evaluation of therapy efficacy are important, and IVCM might enable earlier detection of medical enchancment at a microscopic degree. Total, IVCM serves as a helpful adjunct within the diagnostic method to corneal ulcers, doubtlessly enabling earlier focused administration and response to therapy.
- References:
- Amescua G, et al. Eye (Lond). 2012;doi:10.1038/eye.2011.316.
- Bakken IM, et al. Ocul Surf. 2002;doi:10.1016/j.jtos.2022.03.002.
- Chidambaram JD, et al. Br J Ophthalmol. 2017;doi:10.1136/bjophthalmol-2016-309656.
- Durand ML, et al. N Engl J Med. 2023;doi:10.1056/NEJMra2216081.
- Jin X, et al. Cornea. 2022;doi:10.1097/ICO.0000000000002912.
- Nielsen E, et al. Case Rep Ophthalmol. 2013;doi:10.1159/000357558.
- Prajna NV, et al. JAMA Ophthalmol. 2013;doi:10.1001/jamaophthalmol.2013.1497.
- Soliman W, et al. Graefes Arch Clin Exp Ophthalmol. 2013;doi:10.1007/s00417-012-2086-5.
- Vaddavalli PK, et al. Ophthalmology. 2011;doi:10.1016/j.ophtha.2010.05.018.
- Venugopal A, et al. Indian J Ophthalmol. 2024;doi:10.4103/IJO.IJO_2794_23.
- For extra data:
- Edited by William W. Binotti, MD, and Julia Ernst, MD, PhD, of New England Eye Heart, Tufts College Faculty of Medication. They are often reached at william.binotti@tuftsmedicine.org and julia.ernst@tuftsmedicine.org.