A 52-year-old man introduced to our orthopedic clinic with an 8-month historical past of a proper distal forearm mass accompanied by extreme ache and right-hand numbness.
He reported paresthesias within the median nerve distribution, vital weak spot and practical impairment. Previous to presentation, the affected person had seen an out of doors orthopedic surgeon who ordered an MRI, which advised a median nerve sheath tumor, although he by no means obtained definitive remedy and had been seen by a number of suppliers.

Supply: Austin Q. Nguyen, MD; Jennifer Liu, MD; and Korsh Jafarnia, MD
The affected person introduced to the ED a number of occasions for extreme forearm ache previous to presenting to our clinic for a second orthopedic opinion. His previous medical historical past was exceptional for high-grade B-cell non-Hodgkin lymphoma, initially involving the left maxillary sinus and left orbit recognized in June 2017. He underwent eight programs of chemotherapy and achieved full medical and hematologic remission, confirmed by PET-CT in 2020. Extra comorbidities included gastroesophageal reflux illness and weight problems (BMI higher than 30 kg/m2).
Medical examination, imaging findings
On examination, the affected person had a palpable, tender, volar distal forearm tender tissue mass with no overlying pores and skin adjustments. He had a optimistic Tinel’s signal over the mass within the median nerve distribution. He additionally had a optimistic carpal compression take a look at and Phalen’s take a look at.

Supply: Austin Q. Nguyen, MD; Jennifer Liu, MD; and Korsh Jafarnia, MD
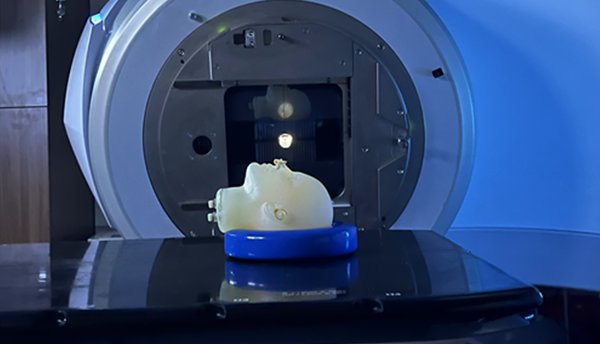
His radial and ulnar pulses have been palpable. An MRI of the fitting distal forearm confirmed an 8.9 cm by 2.4 cm heterogeneous tender tissue mass alongside the course of the median nerve suggestive of a nerve sheath tumor per an out of doors radiology report (Determine 1).
What are the most effective subsequent steps in administration of this affected person?
See reply beneath.
Open carpal tunnel launch with open biopsy
The affected person underwent open carpal tunnel launch with biopsy vs. resection of the forearm mass. The choice for surgical procedure was made primarily based on the affected person’s extreme ache and compressive median nerve signs. MRI findings did favor an encased mass suggestive of peripheral nerve sheath tumor, which if benign, could be resected.
Intraoperatively, the limb was elevated with out exsanguination, and a tourniquet was inflated to 250 mm Hg. A longitudinal incision was revamped the mass and distally alongside the thenar crease for carpal tunnel publicity. The carpal tunnel was launched in an open method, revealing his median nerve was beneath vital pressure. Proximally, fascia overlying the forearm musculature was launched on account of tightness brought on by the mass impact.

Supply: Austin Q. Nguyen, MD; Jennifer Liu, MD; and Korsh Jafarnia, MD
The tumor prolonged roughly 15 cm proximally, positioned beneath the flexor digitorum superficialis muscle, which was fastidiously mobilized utilizing intermuscular planes with out muscle breach (Determine 2). The mass appeared heterogeneous and agency, inconsistent with typical schwannoma options, and couldn’t be shelled out. Tissue samples have been despatched for intraoperative frozen part and pathology. The pathologist famous options according to lymphoma cells, necessitating additional tissue sampling and cytologic analysis. The wound was closed and extra requested tissue samples have been despatched for pathology.
Postoperative course
The affected person tolerated the process nicely, with discount in ache and enchancment in median nerve compressive signs postoperatively. Ultimate pathology and stream cytometry confirmed prognosis of enormous CD5-positive B-cell lymphoma. The affected person was promptly referred again to oncology and seen inside 2 days postoperatively.
Extra oncologic staging/grading work-up was initiated. Given the favorable response of lymphoma to chemoradiotherapy, he started mixed chemo-radiation remedy as soon as his forearm incision was well-healed, 2 weeks postoperatively.
Dialogue
This case highlights a uncommon however essential reason for median nerve compression from recurrent extranodal non-Hodgkin lymphoma. Peripheral nerve compression by extranodal lymphoma is an exceedingly uncommon presentation of non-Hodgkin lymphoma, and just a few circumstances have been reported within the literature. Non-Hodgkin lymphoma usually presents with lymphadenopathy or systemic signs, however extranodal illness does account for as much as 50% of all shows, most regularly involving the gastrointestinal tract, pores and skin, bone marrow and central nervous system. Involvement of peripheral tender tissue buildings reminiscent of muscle tissues or fascial compartments, notably resulting in localized compressive neuropathy, is extraordinarily unusual and could also be simply misdiagnosed. In a 2022 narrative assessment of uncommon tumors inflicting median nerve compression, 94 research have been reviewed and just one case of non-Hodgkin lymphoma was reported.
Franck Marie Leclère, MD, PhD, and colleagues described a affected person case with non-Hodgkin lymphoma involving the flexor digitorum superficialis muscle, which was compressive to the median nerve within the distal forearm. The affected person had electrodiagnostic testing according to carpal tunnel syndrome and underwent carpal tunnel launch at a non-public hand heart leading to unfavorable development of illness. Just like our case, the prognosis was not made till subsequent MRI was carried out adopted by a surgical biopsy, underscoring the problem in preoperative identification, particularly when diagnostic research might counsel benign pathologies.
Our case presents a singular state of affairs of recurrent giant B-cell non-Hodgkin lymphoma involving the deep flexor compartment of the forearm and compressing the median nerve. The affected person’s presentation was additional difficult by an out of doors radiologic interpretation suggesting a benign median nerve sheath tumor, which led to delay in care. It was solely after a number of ED visits and eventual referral to our orthopedic clinic that biopsy and additional administration was explored for the affected person.
Intraoperatively, the atypical options of the mass — heterogeneous look, poorly circumscribed margins and deep location beneath the flexor digitorum superficialis — raised concern for malignancy, prompting an intraoperative frozen part for expedited pathology assessment. Early involvement of pathology allowed for well timed identification of a recurrent non-Hodgkin lymphoma, facilitating a speedy transition to oncologic care. The choice to carry out an open carpal tunnel launch concurrently offered symptomatic reduction for median nerve compression, which is a key studying level from this case.
This case highlights a number of vital issues for clinicians: first, the significance of sustaining a broad differential prognosis when evaluating tender tissue lots, notably in sufferers with a historical past of malignancy; second, the constraints of radiographic imaging alone in diagnosing nerve-adjacent tumors; and third, the therapeutic and diagnostic worth of early surgical exploration and biopsy in ambiguous or progressive circumstances.
In contrast to most peripheral nerve tumors reminiscent of schwannomas or neurofibromas, lymphoma shouldn’t be amenable to easy resection. Its administration depends on correct histopathologic prognosis adopted by systemic remedy. Immediate surgical intervention on this case was essential not just for neurologic restoration but in addition for enabling early tissue prognosis and oncologic referral.
To our information, this is among the few reported circumstances of non-Hodgkin lymphoma presenting as a solitary extranodal forearm mass inflicting remoted median nerve compression with out indicators of systemic recurrence evident at preliminary presentation. Our case reinforces the function of orthopedic surgeons in recognizing uncommon shows of malignancy, facilitating a immediate needle or open biopsy for additional diagnostic data and, finally, coordinating multidisciplinary care to supply high-quality affected person care.
Key factors:
- Non-Hodgkin lymphoma can current as an extranodal peripheral tender tissue mass in muscle or fascial layers inflicting nerve compression and shouldn’t be mistaken for a benign nerve sheath tumor.
- Sufferers with prior lymphoma and new peripheral lots require immediate biopsy to substantiate prognosis.
- Recognizing atypical options of lesions and having a low threshold for early biopsy can expedite multidisciplinary coordination of care in sufferers with malignant tender tissue lots.
References:
For extra data:
Korsh Jafarnia, MD; Jennifer Liu, MD; and Austin Q. Nguyen, MD, could be reached on the division of orthopedics and sports activities drugs at Houston Methodist Hospital in Houston, Texas. Nguyen’s electronic mail: aqnguyen@houstonmethodist.org.
Edited by Mitchell F. Bowers, MD, and Jennifer Liu, MD. Bowers is a chief resident in orthopedic surgical procedure at Vanderbilt College Medical Heart. He will likely be pursuing a backbone surgical procedure fellowship on the Leatherman Backbone Institute following residency completion. Liu is a chief resident in orthopedic surgical procedure at Houston Methodist Hospital. She will likely be pursuing an grownup reconstruction fellowship on the College of California San Francisco following residency completion. For extra data on submitting Orthopedics As we speak Grand Rounds circumstances, please electronic mail orthopedics@healio.com.