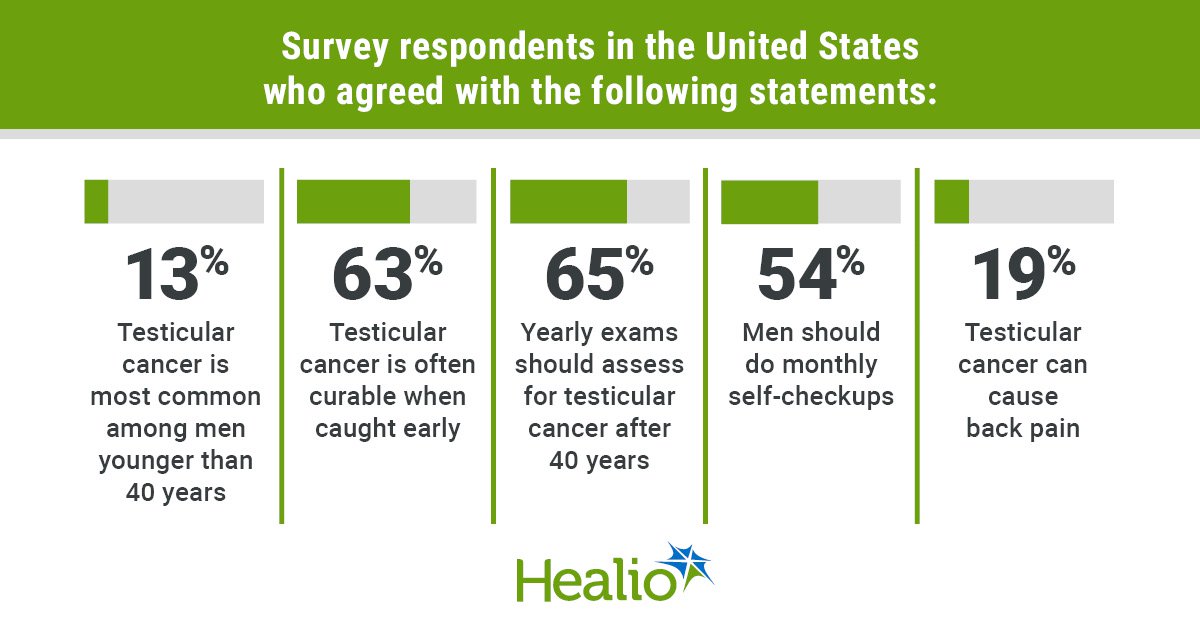
Key takeaways:
- Hospital participation in BPCI Superior lowered whole episode spending for outpatient surgical procedure.
- Inpatient procedures weren’t related to differential modifications in whole episode spending or readmissions.
Bundling funds for outpatient spinal surgical procedure was related to reductions in value and fewer readmissions, in accordance with information reported on the American Affiliation of Neurological Surgeons Annual Scientific Assembly.
“This examine is likely one of the first to judge value-based care (particularly bundled funds) for outpatient surgical procedure,” Grace Y. Ng, MD, MS, neurosurgery resident at Massachusetts Normal Hospital, instructed Healio.

Knowledge have been derived from Ng GY, et al. Financial savings related to bundled funds for outpatient and inpatient backbone surgical procedure episodes. Introduced at: American Affiliation of Neurological Surgeons; April 25-28, 2025; Boston.
“There was an rising shift from inpatient to outpatient surgical procedure and it is very important perceive how well being techniques are adapting to this variation and dealing to enhance worth on this setting,” Ng stated.
In 2018, CMS launched Bundled Funds for Care Enchancment – Superior (BPCI Superior), the primary episode-based fee mannequin to incorporate spinal surgical procedure as an outpatient situation.
Ng and colleagues sought to investigate spending and high quality for outpatient in contrast with inpatient surgical bundles and to find out if hospital participation in BPCI Superior for outpatient and inpatient backbone surgical procedure (again and neck besides spinal fusion procedures, BNESF) was related to modifications in spending and high quality.
Their retrospective observational examine culled information from Medicare claims and differences-in-differences evaluation adjusting for affected person and market traits. A complete of 14,280 people who acquired outpatient BNESF and 23,400 sufferers who acquired inpatient BNESF between 2013 and 2019 at hospitals that participated in BPCI Superior have been paired with a matched comparability cohort of sufferers at non-participating hospitals.
The examine’s main consequence was whole episode spending, together with prices incurred for the index process and 90-day follow-up interval, whereas secondary outcomes included 90-day readmissions, ED visits and total mortality.
Ng and colleagues reported that hospital participation in BPCI Superior was related to a differential discount in whole episode spending (-$1,201 [95% CI: -2,184 to -219]) and readmissions (-2.2 proportion factors [95% CI: -4.2 to -0.1) for outpatient BNESF.
Conversely, for inpatient BNESF, hospital participation in BPCI Advanced was not associated with differential changes in total episode spending or readmissions.
Data additionally showed no significant changes for ED visits or mortality for either group.
“We found that hospitals participating in bundled payments for outpatient surgery achieved reductions in cost and readmissions,” Ng told Healio. “This is an exciting finding that suggests value-based care initiatives may be effective not only for inpatient, but also outpatient surgical settings.”
For more information:
Grace Y. Ng, MD, MS, can be reached at neurology@healio.com.