Hemodialysis is the predominant modality of kidney substitute remedy worldwide.
In the USA, tunneled dialysis catheters stay broadly prevalent, with greater than 80% of sufferers with end-stage kidney illness initiating hemodialysis with a catheter, and about 18% to twenty% nonetheless utilizing catheter past 3 months.
Catheters are additionally probably the most prevalent entry for hemodialysis globally. Catheter-related infections are widespread, usually related to bloodstream infections, one-third of which happen inside the first month of catheter insertion (Massey Ok, et al. Poster introduced at: American Society of Nephrology Kidney Week; Nov. 3-6, 2022; Orlando).
Catheter-related bloodstream infections are related to increased mortality, longer inpatient stays and elevated well being care bills. Thus, it is a crucial objective to reduce incidence of those infections.
Widespread strategies to lower infections in tunneled dialysis catheters embrace most barrier precautions through the insertion and manipulation of catheters throughout dialysis therapies, in addition to correct dressing strategies through the interdialytic interval. Use of antimicrobial-coated catheters, caps and intracatheter units and antimicrobial catheter lock options have emerged in newer occasions.
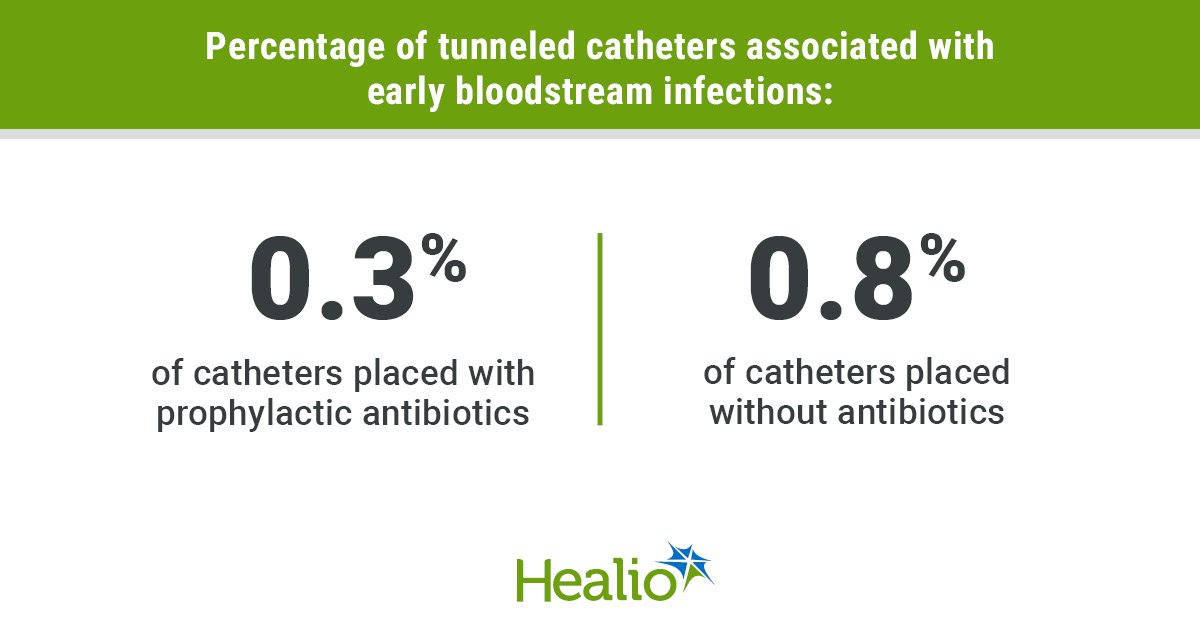
It’s tempting to make use of prophylactic antibiotics previous to catheter insertion to cut back the incidence of early infections after the process. The examine by Lazarus and colleagues examined whether or not systemic antibiotic administration would end in discount of early episodes of hemodialysis catheter-related bloodstream infections within the REDUCCTION trial. This was a nationwide observational cohort examine performed in one among 37 Australian nephrology providers between 2016 and 2020. The authors concluded the percentages of early infections in providers that routinely used systemic prophylactic antibiotics on the time of insertion weren’t considerably totally different to the percentages in providers that didn’t use prophylactic antibiotics.
The examine gives a big perception into the problem of antibiotic prophylaxis after catheter placement to cut back early hemodialysis catheter-related bloodstream infections in a big cohort in Australia. The examine had limitations, which had been acknowledged by the authors, together with nonrandomization of the intervention, small variety of goal occasions and nongeneralizability to different populations. The authors famous that as a result of lower than 1% fee of infections inside 14 days of insertion, it will want an exceptionally giant randomized managed trial to point out a distinction in an infection incidence by utilizing routine antibiotic prophylaxis. Additional, it’s believable that routine use of antibiotics would improve the incidence of antagonistic results, well being care prices and emergence of antibiotic resistance. This apply would immediately contradict the targets of antimicrobial stewardship.
As an interventional nephrologist, I by no means used antibiotic prophylaxis for tunneled dialysis catheter insertion and didn’t encounter greater than a uncommon an infection, which was attributed to improper dealing with of the catheter.
So, what ought to a practitioner do to cut back catheter-related bloodstream infections? The best methodology can be to cut back the variety of catheters used. Catheter discount has remained a frightening objective to realize, regardless of a rise in arteriovenous fistula prevalence.
Can routine antibiotic prophylaxis cut back the numbers of early infections? Within the absence of appropriately carried out giant trials, it is very important critically contemplate the dangers and advantages, particularly when the charges of an infection have declined considerably within the final decade. Between 2014 and 2019, bloodstream an infection charges in hemodialysis decreased by 40% total (Keenan J, et al. Clin J Am Soc Nephrol. 2024;doi:10.2215/CJN.0000000000000476). On this interval, catheter-related bloodstream an infection fee decreased from 2.16 per 100 patient-months in 2014 to 1.21 per 100 patient-months in 2019.
Along with aware efforts by all stakeholders to implement extra stringent an infection management practices, a number of advances in an infection prophylaxis in dialysis items might have been answerable for the discount. Use of newer catheter caps, intracatheter units and an FDA-approved antimicrobial catheter lock resolution are prone to maintain, and even additional cut back, the charges in future.
In consideration of those advances, the apply of routine antibiotic prophylaxis to cut back early catheter-related bloodstream infections shouldn’t be solely unproven, expensive and related to potential unintended effects, together with bacterial resistance, however it’s also pointless and must be discouraged.
Anil Ok. Agarwal, MD, FACP, FASN, FNKF, FISN, FASDIN
Disclosures: Agarwal studies being a professor on the College of California, San Francisco, and has an editorial function in lots of journals together with Journal of Vascular Entry. Agarwal is a guide to AstraZeneca, Cormedix and Pfizer.