If it has appeared like extra individuals you already know are creating diabetes, you might be proper. The diabetes epidemic just isn’t known as an epidemic for nothing: In keeping with the American Diabetes Affiliation, over 10% of the U.S. inhabitants—roughly 38.4 million individuals—had diabetes in 2021, and 1.2 million extra individuals get identified annually.
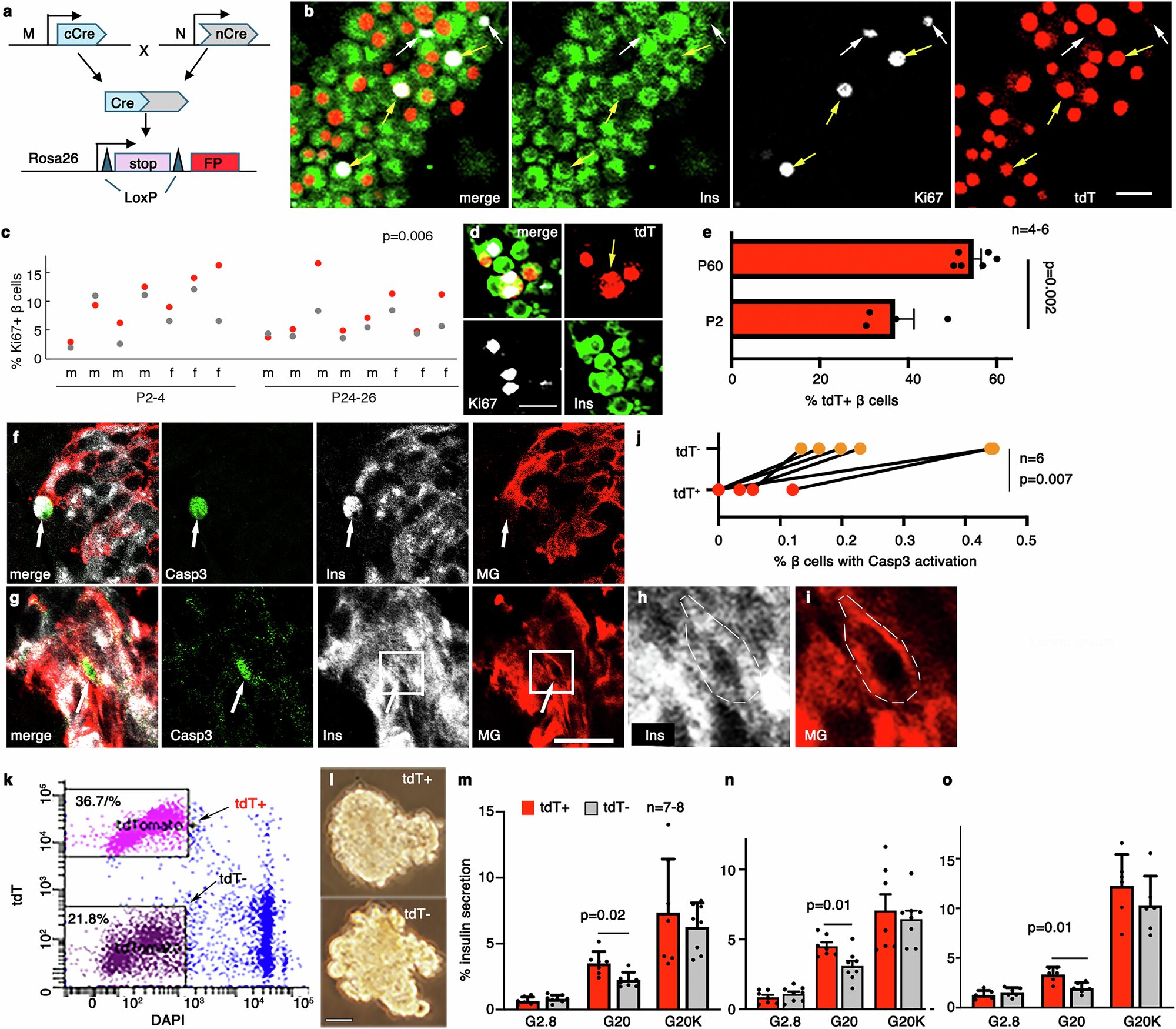
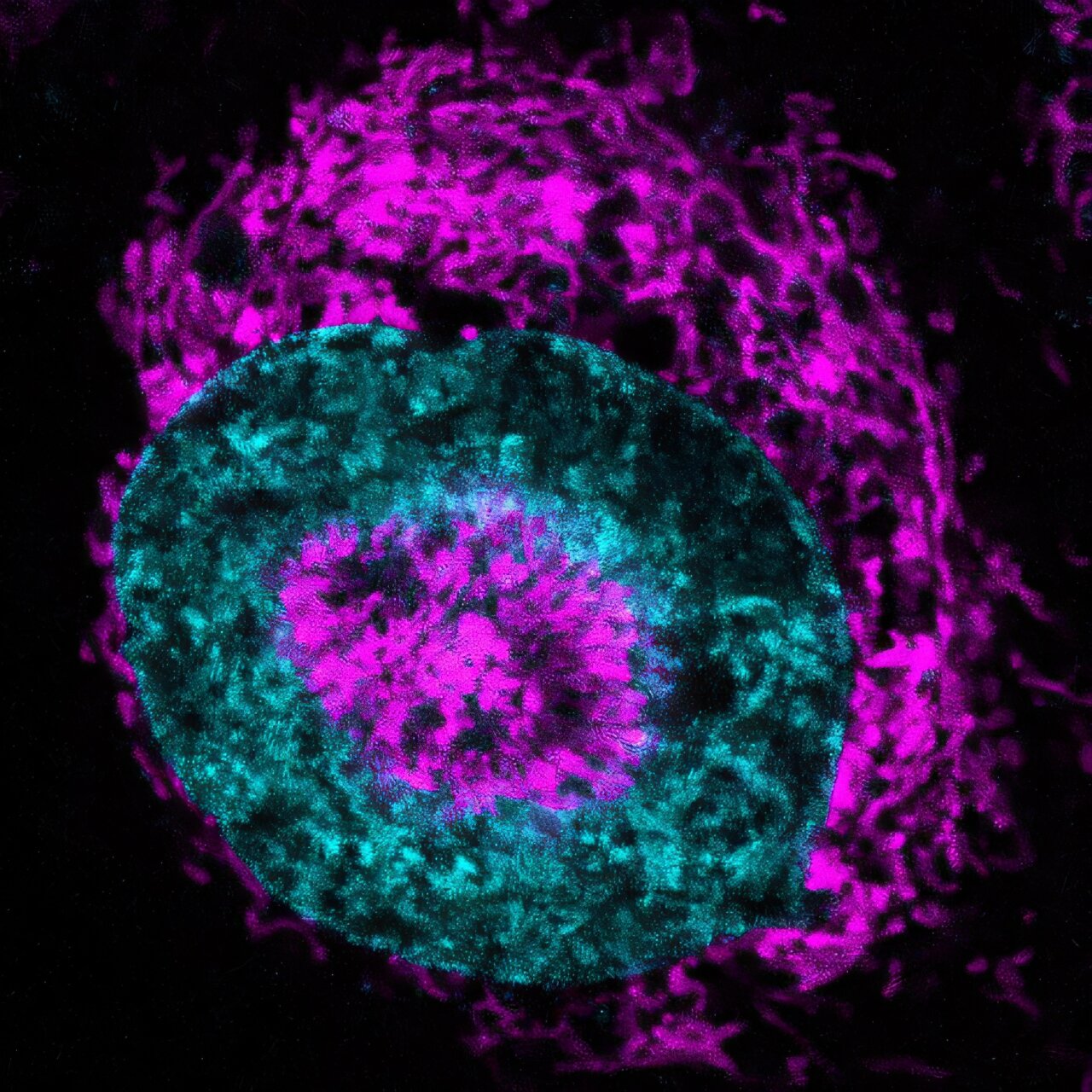
Sort 2 diabetes happens when your physique develops a resistance to insulin, the hormone that helps regulate glucose ranges in your blood. Insulin is secreted by pancreatic cells known as β-cells, and in T2D, they ramp up insulin manufacturing to attempt to regulate blood glucose ranges, however even that’s inadequate and the β-cells ultimately turn into exhausted over time. Because of their significance, the purposeful β-cell mass, or the entire variety of β-cells and their operate, determines an individual’s danger of diabetes.
Β-cells are usually not homogeneous, even inside a single particular person, and consist of various “subtypes,” every with their very own secretory operate, viability, and talent to divide. In different phrases, every β-cell subtype has a unique degree of health, and the upper, the higher. When diabetes develops, the proportions of some β-cell subtypes are modified. However a key query stays: Are the proportion and health of various β-cell subtypes altered by diabetes or are the modifications chargeable for the illness?
Cue Guoqiang Gu, Emily Hodges, and Ken Lau, Vanderbilt college members who got down to reply these questions, and extra. Their current work, printed in Nature Communications, is a step towards figuring out whether or not it’s attainable to reinforce purposeful β-cell mass to cut back the danger of T2D. Gu and Lau are professors of cell and developmental biology and Hodges is an affiliate professor of biochemistry.
Finding out β-cell subtypes is difficult. The commonest technique of finding out them known as “terminal examination of samples at single-cell ranges,” which signifies that scientists can solely research explicit β-cell subtypes as soon as, and solely when they’re absolutely developed, which precludes them from inspecting a particular cell subtype at distinct levels in differentiation, maturation, proliferation, senescence, demise, and extra. If they might monitor β-cells at a number of levels, researchers may higher perceive how cells’ states drift over time or beneath completely different physiological situations.
Gu, Hodges, and Lau developed a technique that avoids this drawback by indelibly marking the progenitor cells that give rise to the β-cell subtypes with completely different gene expression combos. The markings enabled the researchers to trace the identical β-cell subtypes over time at completely different levels, permitting them to sort out questions on β-cell subtypes with confidence.
The analysis paper yielded three major outcomes:
- Progenitor cells that give rise to β-cells with completely different gene expression markers in embryonic mice give rise to β-cell subtypes with various ranges of health in grownup mice. This helps researchers perceive how completely different β-cell subtypes come up and will assist them sooner or later manipulate progenitor cells to favor sure subtypes over others and reduce the danger of diabetes.
- The vitamins that mom mice eat have a transparent impact on the proportion of high-fitness to low-fitness β-cell subtypes of their pups. For instance, when mom mice had been on a high-fat weight loss plan and overweight, their pups had fewer β-cells that responded higher to glucose ranges. What this mannequin for weight problems exhibits is that maternal weight problems will increase the danger of diabetes for the offspring. This provides scientists and clinicians a greater understanding of the hereditary components and maternal medical historical past that may predispose somebody to diabetes.
- The β-cell subtypes recognized in mice have parallels within the human pancreas. In actual fact, the β-cell subtype predicted to have larger health in people was noticed to be diminished in sufferers with T2D. Though the findings from animal research are usually not at all times straight relevant to people and human well being, these outcomes recommend that β-cell subtypes in mice might be useful for understanding human biology and the danger of diabetes.
The researchers now hope to discover how the epigenetic patterns (the gene expression markers talked about above) are constructed and maintained within the completely different β-cell subtypes and the way disturbing these patterns impacts β-cell health.
“Because of this and different analysis, it might be attainable to sooner or later create a weight loss plan complement for being pregnant that might cut back the danger of diabetes for infants,” Gu mentioned.
Extra questions stay unanswered that tie into potential diabetes therapies: does modulating DNA methylation (an epigenetic marker) enhance the purposeful high quality of human embryonic stem cell–derived, β-like cells? If that’s the case, can these β- and β-like cells be used for transplantation-based diabetes therapies by which T2D sufferers obtain β-cells of upper health?
These questions stay to be explored.
Extra info:
Monica E. Brown et al, Pancreatic islet β-cell subtypes are derived from biochemically-distinct and nutritionally-regulated islet progenitors, Nature Communications (2025). DOI: 10.1038/s41467-025-60831-0
Quotation:
New findings reveal how β-cell subtypes affect kind 2 diabetes growth (2025, July 29)
retrieved 29 July 2025
from https://medicalxpress.com/information/2025-07-reveal-cell-subtypes-diabetes.html
This doc is topic to copyright. Aside from any honest dealing for the aim of personal research or analysis, no
half could also be reproduced with out the written permission. The content material is offered for info functions solely.