Key takeaways:
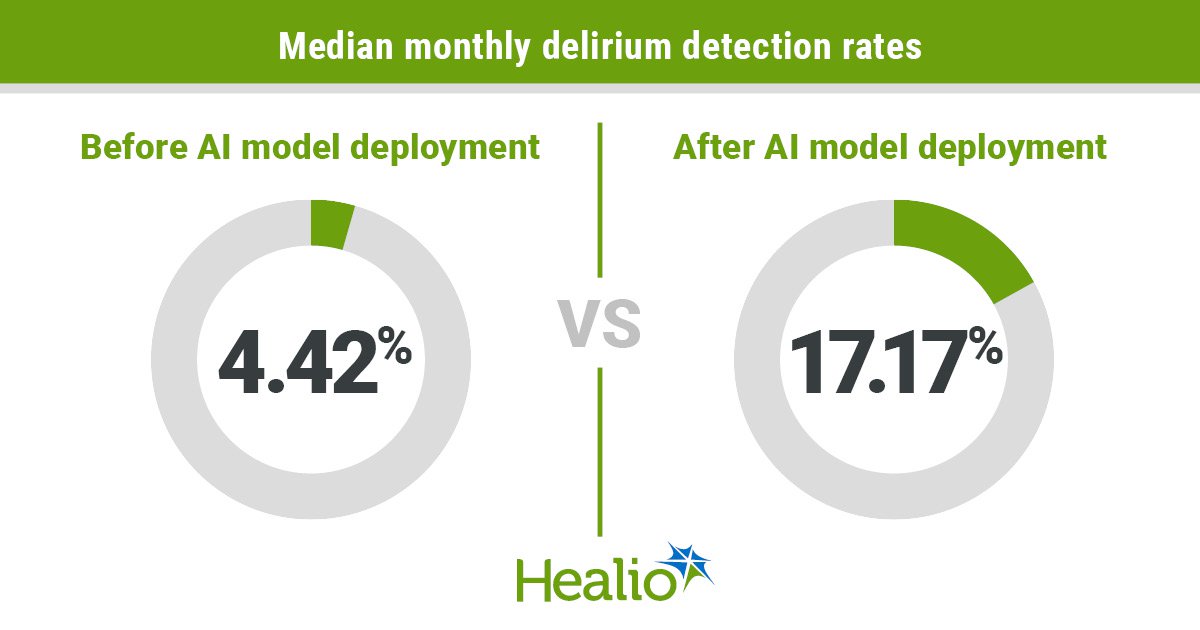
- Use of an AI mannequin resulted in a virtually fourfold improve in delirium circumstances detected amongst hospitalized older adults.
- The mannequin, which didn’t require further screening time, allowed for earlier intervention.
An AI mannequin designed to automate evaluation of delirium danger elevated the variety of detected circumstances amongst hospitalized older adults, in accordance with outcomes of a top quality enchancment examine.
Use of the mannequin, which alerts skilled group members to evaluate sufferers deemed at excessive danger, resulted in 4 instances as many delirium circumstances recognized in contrast with customary approaches with out growing time required for screening.

Knowledge derived from Friedman JI, et al. JAMA Netw Open. 2025;doi:10.1001/jamanetworkopen.2025.8874.
The mannequin — evaluated for people with quite a lot of diagnoses, together with most cancers — additionally allowed for earlier intervention, reminiscent of decreasing use of doubtless inappropriate drugs.

Joseph I. Friedman
“That is clinically significant on various ranges,” researcher Joseph I. Friedman, MD, founder and director of delirium providers for Mount Sinai Well being System and professor of psychiatry and neuroscience at Icahn College of Medication at Mount Sinai, instructed Healio.
“To extend detection of a really severe situation — which is related to many short- and long-term adverse penalties — is large. Past the advantages for sufferers, this helps our employees by liberating up their time, permitting them to ship extra environment friendly and impactful well being care to those that want it most.”
Healio spoke with Friedman and two different clinicians — an internationally acknowledged thought chief in delirium analysis, in addition to a medical oncologist and palliative care specialist who has studied agitated delirium amongst folks with most cancers — concerning the challenges related to delirium detection, how AI might assist scale back the variety of circumstances which might be ignored in medical care, and the necessity for personalised administration as soon as delirium is identified.
An underdiagnosed syndrome
As much as one-third of hospitalized people develop delirium, the fast onset of confusion or adjustments in psychological standing that have an effect on an individual’s consciousness or capability to focus.
The situation — related to extended hospital stays, long-term practical or cognitive decline and higher want for expert nursing care after hospitalization — typically goes undetected.
“Delirium will not be a single medical entity. It’s extra of a syndrome, so you’ll be able to’t rely on one attribute kind of presentation,” Friedman stated.
Hyperactive delirium — essentially the most acknowledged type — could also be characterised by agitation so excessive that sufferers interact in behaviors dangerous to themselves or employees.
Hypoactive delirium is way much less apparent.
“These sufferers could possibly be torpid or sleep many of the day. They’re not making issues for anyone,” Friedman stated. “They’re very confused, however they’ve fewer delusions or hallucinations than sufferers with the hyperactive type, so they have an inclination to fly beneath the radar.”
Delirium is the commonest neuropsychiatric complication noticed amongst people with most cancers.
It is also essentially the most difficult, in accordance with David Hui, MD, MSc, FAAHPM, director of supportive and palliative care analysis at The College of Texas MD Andrson Most cancers Heart.

David Hui
“Most cancers care requires many complicated selections that depend on real-time enter from sufferers,” Hui, who was not concerned within the examine, instructed Healio. “As a result of delirium impacts the affected person’s thoughts, it impacts our capability to evaluate signs, to speak with them successfully and to debate therapy choices. It’s a very distressing syndrome that may have an incredible affect on the affected person, their caregivers and the well being care system, given delirium’s affiliation with longer hospital stays and better danger for mortality.”
Systematic and longitudinal screening is good, however that usually doesn’t occur in observe.
Many establishments lack the sources to carry out formal assessments on all hospitalized sufferers.
Delirium additionally is often mistaken for different situations, reminiscent of nervousness or insomnia, Hui stated.
“That ends in missed alternatives for detection and intervention, so there undoubtedly is extra work to do,” Hui instructed Healio.
Extra return on funding
AI-based approaches for delirium danger evaluation have proven promise in laboratory settings, however they haven’t carried out as effectively in medical observe.
Friedman and colleagues developed a mannequin that makes use of machine studying to determine patterns in digital medical document knowledge that correlate with delirium danger. The mannequin additionally incorporates pure language processing that identifies patterns in staff-written chart notes, together with observations about refined adjustments in a affected person’s psychological standing.
“Medical decision-support instruments typically are developed in sterile knowledge ecosystems. Archival affected person knowledge are used to create a mannequin that will get handed to clinicians and different hospital personnel to implement, they usually’re instructed, ‘Discover a method to make use of this,’” Friedman stated.
“In our case, we began out with an issue: We spent a lot time doing delirium assessments however, for each 100 sufferers we screened, solely 4 or 5 can be optimistic,” he added. “We wanted to provide you with a technique to give us extra return on our funding of time, permitting us to determine sufferers at biggest danger so we may direct our extremely developed sources to the suitable sufferers, at once, and help our employees by liberating them as much as ship extra environment friendly well being care.”
Researchers adopted a vertical integration strategy, which allowed them to coach, take a look at and refine the mannequin in actual time inside a medical setting to make sure effectiveness and practicality.
Their evaluation included knowledge from 32,284 sufferers aged 60 years or older (imply age, 73.5 years; 53.1% males) admitted to non-ICU models at The Mount Sinai Hospital. Sufferers had a broad vary of medical or surgical major diagnoses, together with most cancers, cardiac situations, gastrointestinal bleeds, or admission for neurosurgery or orthopedic procedures.
The bulk (n = 25,261) comprised the cohorts used for mannequin coaching and testing or reside medical deployment validation.
The remaining subgroup (n = 7,023) included sufferers admitted earlier than and after deployment of the mannequin in observe who underwent delirium danger stratification with the Confusion Evaluation Technique (CAM), a standardized instrument that assesses the presence, severity and fluctuation of 9 delirium options. This allowed for retrospective evaluation of the mannequin’s results on workflow and medical outcomes.
Key outcomes included space beneath the receiver working attribute curve (AUROC), month-to-month charges of delirium detection and median size of hospital keep. Investigators additionally assessed every day doses of opiate, benzodiazepine and antipsychotic drugs.
Delirium charges
Knowledge from the mannequin validation in reside medical observe confirmed an AUROC of 0.94 (95% CI, 0.93-0.95).
An evaluation of inpatients assessed for delirium with CAM confirmed use of the AI mannequin led to a fourfold improve in median month-to-month delirium detection charges, from 4.42% (95% CI, 3.7%-5.14%) earlier than mannequin deployment to 17.17% (95% CI, 15.54%-18.8%) after (P < .001).
Researchers additionally reported lowered doses of sedative drugs with recognized delirium-inducing results after mannequin deployment.
Median every day doses of benzodiazepines declined from 1.6 diazepam dose equivalents (interquartile vary [IQR], 0.66-4.27) earlier than mannequin deployment to 0.93 (IQR, 0.42-2.28) after. Median every day doses of olanzapine, an antipsychotic, declined from 2.5 mg (IQR, 1.16-6.65) earlier than to 1.09 mg (IQR, 0.38-2.46) after (P < .001).
Outcomes confirmed considerably longer median size of keep within the post-machine studying cohort (13.11 days vs. 6.78 days). Researchers attributed this to the upper prevalence of delirium and better Elixhauser Comorbidity Index.
Knowledge generalizability, interpretation
The findings reveal the potential for AI to help delirium danger stratification, however questions stay concerning the applicability of this strategy to different establishments, in accordance with Edward R. Marcantonio, MD, SM, part chief for analysis within the division of common drugs at Beth Israel Deaconess Medical Heart and professor of medication at Harvard Medical College.

Edward R. Marcantonio
“This high quality enchancment challenge was carried out on the fundamental Mount Sinai hospital, however there could possibly be nuances within the knowledge which might be idiosyncratic to that hospital that restrict generalizability to different hospitals,” Marcantonio, who was not concerned with the examine, instructed Healio. “How effectively does this work at different hospitals, or does each hospital should develop its personal algorithm?”
The mannequin has been built-in into operations at The Mount Sinai Hospital. Deployment to Mount Sinai affiliate hospitals is underway.
Friedman acknowledged further validation at different hospital programs — significantly people who don’t have devoted delirium providers — will likely be essential to assess the mannequin’s efficiency and decide if changes are wanted.
“Our hope is to alter the usual of observe, or at the very least contribute to it not directly,” Friedman stated. “This mannequin doesn’t concentrate on one prognosis or one kind of affected person, so our hope is that will probably be straightforward to scale to different hospital programs.”
Hui famous caveats that he stated might restrict how the information might be interpreted, starting with methodologic issues.
The CAM rating is “very effectively established and extensively accepted,” Hui stated.
The delirium detection price within the examine was calculated because the ratio of CAM-positive delirium screening outcomes to complete CAM assessments carried out.
“Within the pre-machine studying cohort, all sufferers with at the very least one CAM rating had been included within the evaluation,” Hui stated. “Within the submit cohort, sufferers recognized by machine studying as being at excessive danger had been prioritized for CAM screening. Variations in traits of who had been chosen for CAM screening within the two cohorts might make it more durable to interpret the findings.
“Delirium is underdiagnosed, and machine studying might increase medical observe by serving to to determine sufferers at excessive danger for delirium, permitting for earlier detection,” Hui added. “Nonetheless, as a result of this was a top quality enchancment challenge and can’t totally management for potential confounders, the query of how we apply it in observe nonetheless wants additional analysis.”
‘AI does the heavy lifting’
Simpler and environment friendly methods are wanted to scale back the variety of delirium circumstances which might be ignored in routine medical care.
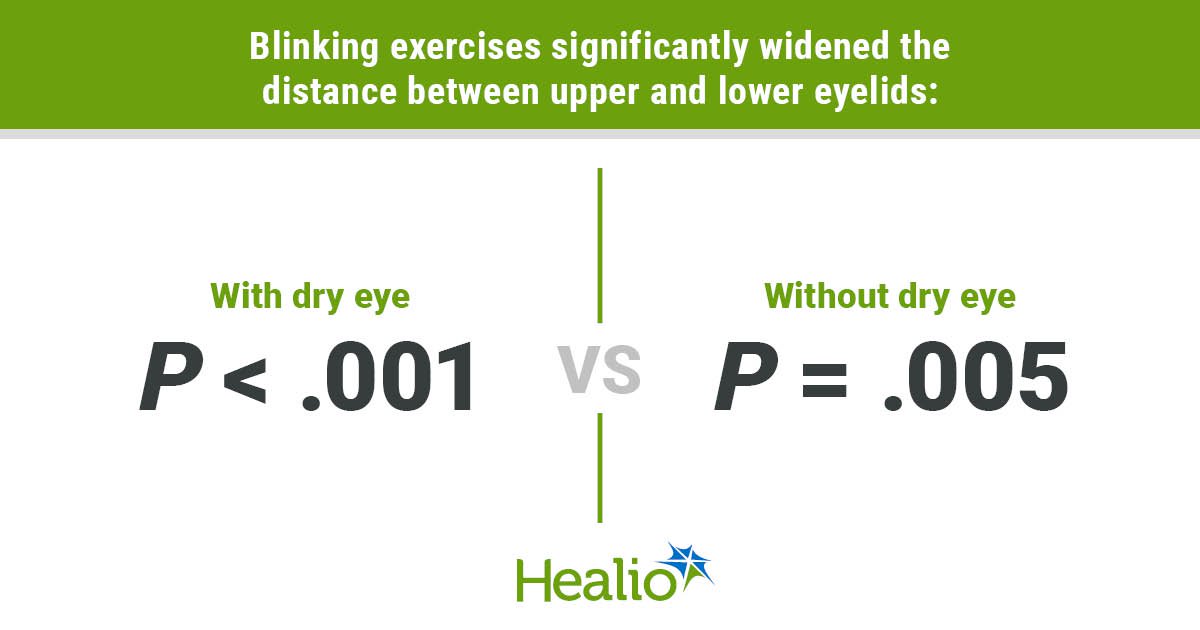
Marcantonio and colleagues developed the Extremely-Temporary Confusion Evaluation Technique, designed to rule out delirium in about 45 seconds. If preliminary screening suggests elevated danger, further questions can decide delirium standing in about 2 minutes. Researchers are testing that strategy now as a part of an NIH examine.
The examine by Friedman and colleagues is an instance of one other common technique — concentrating on people on the highest danger.
“Delirium fluctuates, so a single screening is inferior to a number of screenings,” Marcantonio instructed Healio. “With this mannequin, the identical affected person may come up repeatedly, and a number of CAMs could possibly be carried out on the identical high-risk affected person. Because the examine confirmed, that can lead to a a lot increased yield than doing many extra CAMs on low-risk sufferers.”
This creates alternatives for earlier intervention.
“That might enable for clinicians to observe sufferers extra intently and search for issues that may contribute to delirium — reminiscent of dehydration — and supply multimodal, nonpharmacologic interventions to stop delirium,” Hui stated. “That’s the supreme state of affairs, as a result of one of the best ways to handle delirium is to stop it.”
In lots of circumstances, nevertheless, delirium can’t be prevented. As soon as identified, administration should be personalised, Marcantonio stated.
“We don’t have a drug to deal with delirium,” he stated. “It’s not like we determine a case, administer one thing and all of it goes away.”
A multipronged strategy is important to determine and deal with potential causes, in addition to handle behavioral points that come up.
It’s important to acknowledge that every case is exclusive, Marcantonio added.
“Some sufferers with delirium have to be calmed down and others have to be activated,” Marcantonio stated. “It actually requires a custom-made therapy plan.”
In broader phrases, the examine findings assist dispel a standard false impression concerning the position of AI in drugs, Friedman stated.
“Relating to making selections about prognosis, therapy or analyzing imaging, AI completely is right here to help us, not exchange us,” Friedman stated. “I may have a group of 10 folks spending their complete day taking a look at charts to find out who’s most in danger for delirium, however the AI does the heavy lifting and takes care of one thing that will eat up all of our time if we did it manually.
“It doesn’t give a definitive prognosis, however it tells us who’s at elevated danger,” he added. “We finally make the prognosis and the therapy plan, however this provides us extra time to concentrate on making these extraordinarily vital selections.”
For extra data:
Joseph I. Friedman, MD, might be reached joseph.friedman@mountsinai.org.
David Hui, MD, MSc, FAAHPM, might be reached at dhui@mdanderson.org.
Edward R. Marcantonio, MD, SM, might be reached at emarcant@bidmc.harvard.edu.