Key takeaways:
- Lengthy-term BP decreasing was not linked to elevated danger for most cancers or cancer-related demise.
- New meta-analysis and Mendelian randomization research “fills … hole in proof” on hyperlink between BP decreasing and most cancers.
Lengthy-term antihypertensive remedy was not related to danger for most cancers, cancer-related mortality or site-specific cancers of any kind, in accordance with research findings.
Utilizing knowledge from greater than 300,000 contributors in 42 randomized managed trials, Milad Nazarzadeh, DPhil, senior analysis fellow in cardiovascular and genetic epidemiology within the Nuffield Division of Girls’s and Reproductive Well being at College of Oxford, U.Ok., and colleagues carried out a meta-analysis to judge whether or not there’s an affiliation between long-term BP decreasing with antihypertensive therapies and danger for most cancers and cancer-related demise.

Lengthy-term BP decreasing was not linked to elevated danger for most cancers or cancer-related demise. Picture: Adobe Inventory
The info had been revealed in JACC: CardioOncology.
“Hypertension, which requires long-term pharmacologic blood pressure-lowering remedy, is essentially the most generally noticed coexisting situation in sufferers with most cancers,” Nazarzadeh and colleagues wrote.
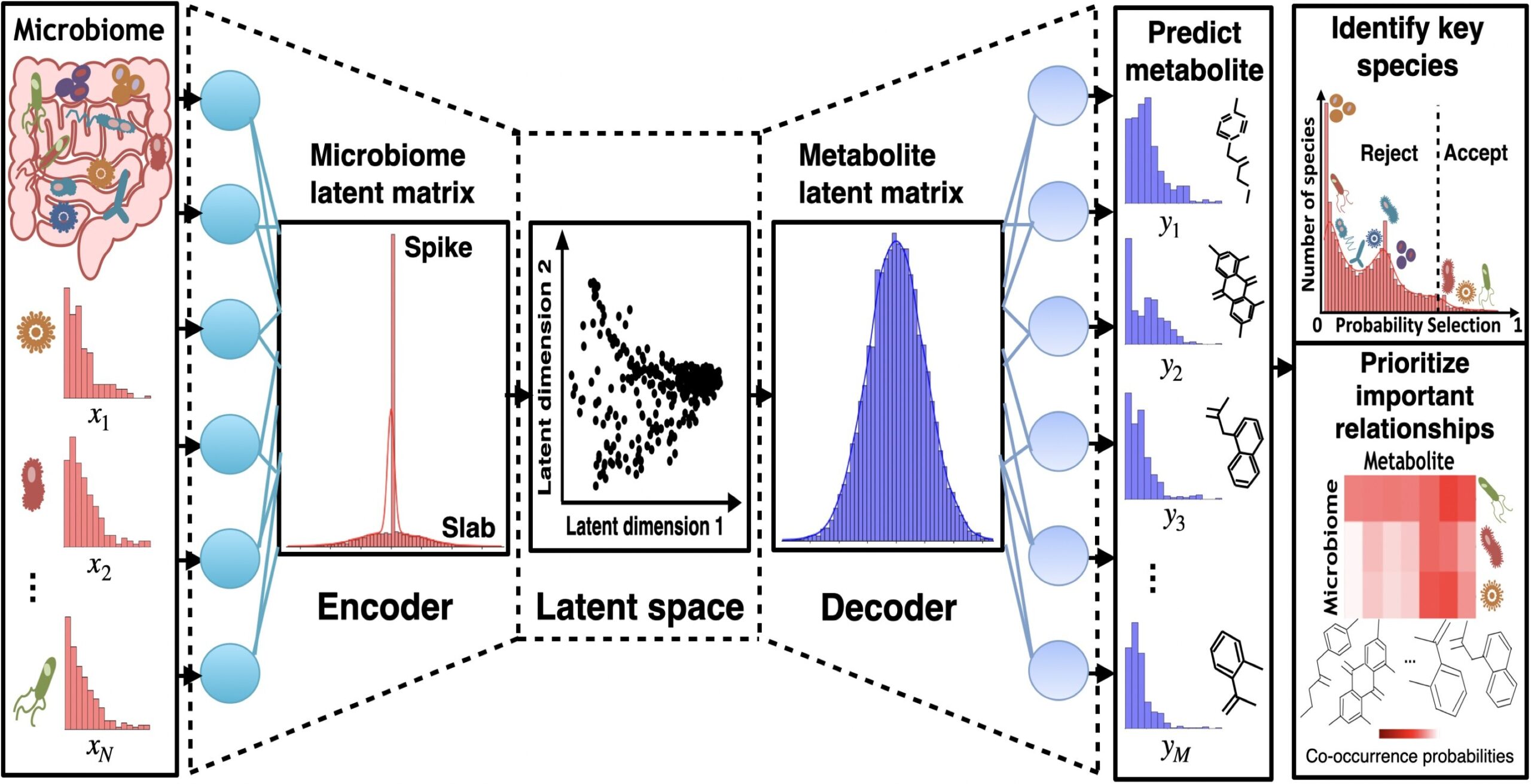
Nazarzadeh and colleagues performed a meta-analysis of particular person participant knowledge from 42 randomized managed trials of pharmacologic BP-lowering interventions and carried out a Mendelian randomization evaluation to judge the results of long-term BP decreasing on site-specific cancers.
Pharmaceutical BP-lowering trials eligible for the meta-analysis included these with at the very least 1,000 participant-years of follow-up in every trial arm and knowledge on most cancers occasions.
The first end result was incident most cancers of any kind. Secondary outcomes had been cause-specific most cancers demise and chosen site-specific cancers.
The meta-analysis included 314,016 contributors assigned to antihypertensive remedy with out recognized most cancers at baseline. Throughout a median follow-up of 4 years, 5.7% of contributors developed most cancers and 1.5% died of most cancers.
The researchers noticed no affiliation between discount in systolic or diastolic BP and most cancers danger (HR per 5 mm Hg discount in systolic BP = 1.03; 95% CI, 0.99-1.06; HR per 3 mm Hg discount in diastolic BP = 1.03; 95% CI, 0.98-1.07) or cancer-related demise (HR per 5 mm Hg discount in systolic BP = 1.03; 95% CI, 0.98-1.1; HR per 3 mm Hg discount in diastolic BP = 1; 95% CI, 0.94-1.07).
There was no vital proof of heterogeneity in danger for any most cancers based mostly on intercourse, age, baseline BP, BMI, smoking standing or historical past of BP-lowering remedy previous to trial randomization (P for all > .22), in accordance with the outcomes.
Equally, the researchers reported no vital affiliation between long-term BP decreasing and cause-specific most cancers demise.
The researchers reported a pattern towards elevated danger for lung most cancers amongst these assigned BP-lowering remedy (RR per 5 mm Hg discount in systolic BP = 1.17; 99.5% CI, 1.02-1.32; RR per 5 mm Hg discount in diastolic BP = 1.17; 99.5% CI, 0.98-1.36). Nevertheless, Mendelian randomization confirmed no affiliation between long-term BP decreasing and site-specific cancers, together with lung most cancers and its subtypes.
“There’s a lack of current proof from [randomized controlled trials] investigating the impact of pharmacologic blood strain decreasing per se on incident most cancers,” the researchers wrote. “Our research fills this hole in proof by pooling individual-level knowledge from randomized trials of blood pressure-lowering remedy. We’ve proven that blood strain decreasing doesn’t impact the chance for incident most cancers or most cancers demise, with no improve or lower throughout follow-up time. The absence of temporal change in relative danger is noteworthy, because it serves as an indicator of the shortage of a causal impact, particularly inside the context of knowledge derived from [randomized controlled trials].”