Key takeaways:
- Sufferers obtained prednisolone or ebastine each day for 7 days throughout tree pollen season.
- Day by day symptom scores and drugs use have been comparable.
- High quality of life scores additionally noticed comparable enhancements.
Prednisolone and antihistamine tablets offered comparable ranges of aid for sufferers with allergic rhinitis throughout tree pollen season, in response to a examine revealed in Medical and Translational Allergy.
These findings underscore the advantages of individualized therapies for sufferers with tree pollen allergy, Carl Skröder, PhD scholar, division of ear, nostril and throat illnesses, division of medical science, intervention and expertise, Karolinska Institutet, and colleagues wrote.

Knowledge have been derived from Skröder C, et al. Clin Transl Allergy. 2024;doi:10.1002/clt2.70017.
The interventional, single-center, double-blind, randomized trial included 18 adults (9 ladies; imply age, 30 years) receiving a 20 mg pill of prednisolone and 16 adults (eight ladies; imply age, 29 years) receiving a 20 mg pill of ebastine every day for 7 days through the finish part of the 2018 tree pollen season.
There have been no vital variations between the teams in each day symptom scores (dSS), each day treatment scores (dMS) or each day mixed symptom and drugs scores (dCSMS), the researchers mentioned.
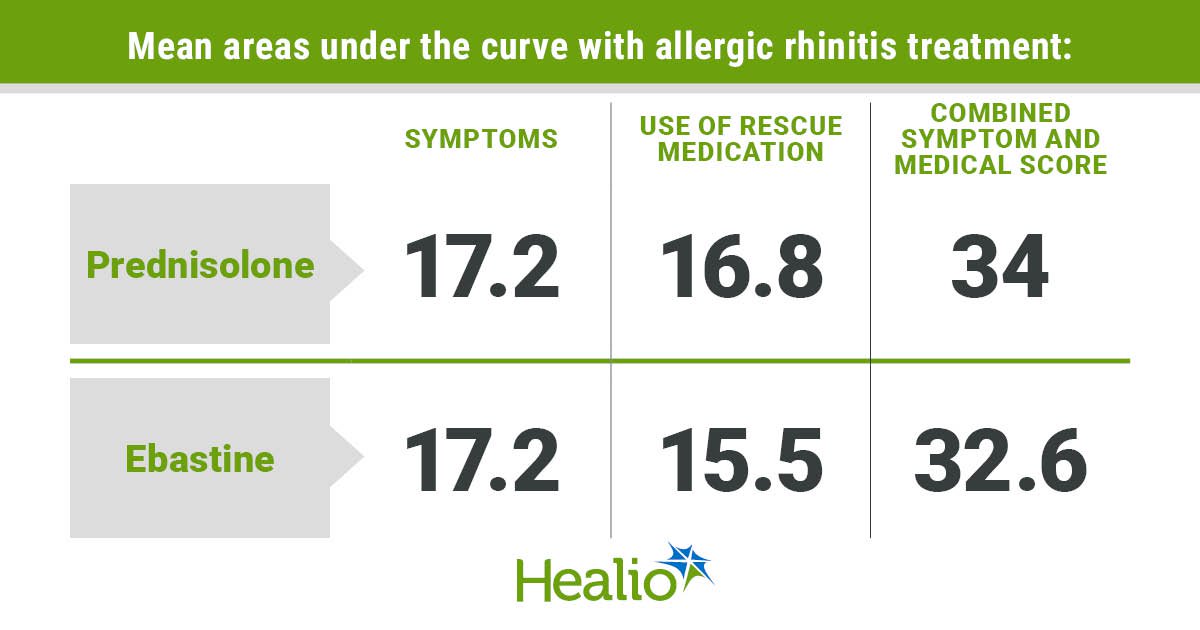
Imply areas underneath the curve (AUCs) for signs included 17.2 (95% CI, 11.7-22.7) for the prednisolone group and 17.2 (95% CI, 13.7-20.5) for the ebastine group.
Imply AUCs for using rescue treatment included 16.8 (95% CI, 12.3-21.2) for the prednisolone group and 15.5 (95% CI, 10.2-20.8) for the ebastine group, which didn’t characterize a big distinction both, the researchers mentioned.
Moreover, imply AUCs included 34 (95% CI, 24.5-43.4) for the prednisolone group and 32.6 (95% CI, 25.6-39.7) for the ebastine group in dCSMS scores, which the researchers referred to as a 4% discount in contrast with the prednisolone group.
Each teams skilled vital decreases in imply 22-item Sino-Nasal Consequence Check scores between days 1 and 21, with a fall from 1.65 to 1.14 (P = .03) for the prednisolone group and from 1.5 to 1.2 (P = .04) for the ebastine group.
At baseline, imply whole SNOT-22 scores included 36.3 for the prednisolone group and 33 for the ebastine group, which the researchers referred to as average. These means fell to 25.1 for the prednisolone group and 26.5 for the ebastine group, with each indicating enchancment, the researchers mentioned.
Imply Juniper Rhinoconjunctivitis High quality of Life Questionnaire (RQLQ) scores considerably fell for each teams between days 1 and 21 as nicely, together with a drop from 2.61 to 1.78 (P = .02) for the prednisolone group and from 2.39 to 1.69 (P = .01) for the ebastine group.
By the top of the examine interval, there have been no vital variations in high quality of life between the 2 teams, which the researchers mentioned may very well be because of decreased pollen counts because the tree pollen season progressed.
Each teams skilled predominantly gentle antagonistic occasions — mostly sneezing, nasal blockage, nasal drip and itching within the nostril and eyes — with no critical antagonistic occasions.
Based mostly on these findings, the researchers concluded that prednisolone didn’t yield any vital discount in signs or treatment use in contrast with antihistamines through the 2018 tree pollen season.
The researchers additionally mentioned these findings present how evidence-based practices and patient-centered care needs to be prioritized in managing allergic rhinitis, with individualized therapy methods tailor-made to affected person preferences and tolerability.