Key takeaways:
- Hospitalized sufferers in 2023 vs. 2014 have been older, extra acutely in poor health and had larger prevalences of a number of comorbidities.
- Vasopressor use and invasive mechanical air flow charges shifted between 2014 and 2023.
SAN FRANCISCO — Amongst ICU sufferers, there was a heightened chance for in-hospital mortality in the course of the COVID-19 pandemic, however after the pandemic, the chances returned to these noticed within the 2010s, in accordance with examine outcomes.
This examine was introduced on the American Thoracic Society Worldwide Convention and printed in JAMA in April.

Knowledge have been derived from Moin EE, et al. Use of life help and outcomes amongst sufferers admitted to intensive care models. AJRCCM, NEJM, JAMA: Discussions on the Edge: Studies of just lately printed important care analysis. Introduced at: American Thoracic Society Worldwide Convention; Could 16-21, 2025; San Francisco.
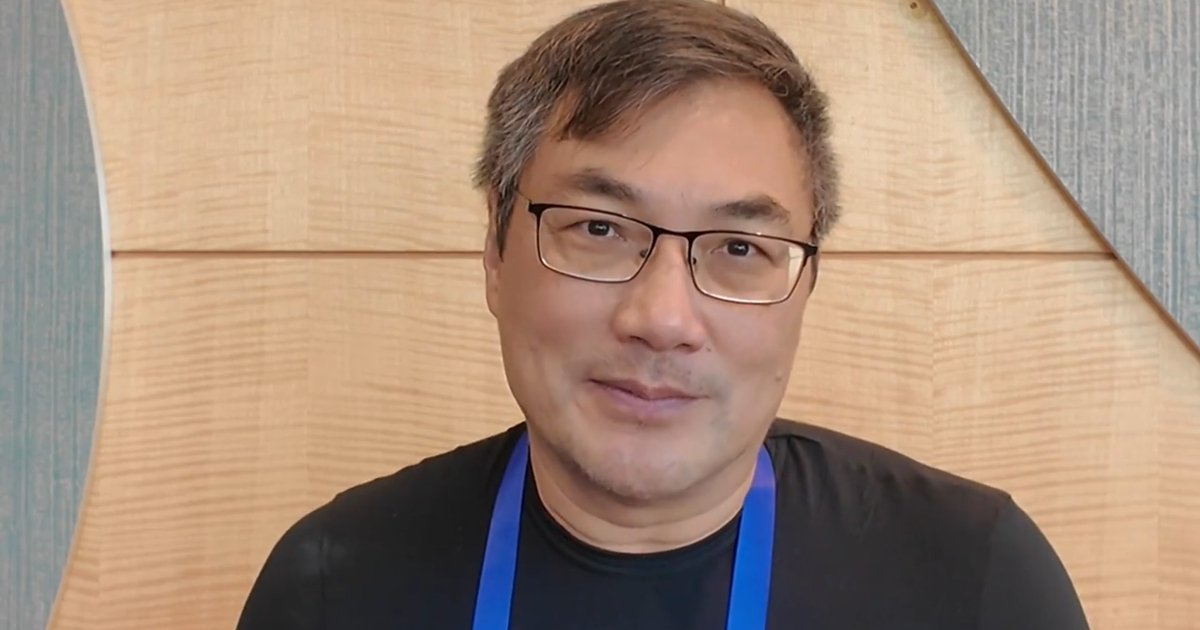
“The period of lowering in-hospital mortality amongst ICU sufferers ended someday round 2014,” Emily E. Moin, MD, MBE, postdoctoral analysis fellow on the College of Pennsylvania, mentioned throughout her presentation.
Between 2014 and early 2020, Moin mentioned, in-hospital mortality was “fairly steady” at 10% to 11%, however that modified as soon as the pandemic started.
Unadjusted information then indicated decreases in in-hospital mortality in late 2022 and 2023 for sufferers who have been each COVID optimistic and COVID detrimental, Moin mentioned.
“Even amongst COVID detrimental sufferers, we see that it didn’t come again all the way down to its pre-pandemic baseline,” she mentioned. “However these are unadjusted information. With a purpose to interpret them, we actually must put them in context with different modifications.”
Utilizing 2014 to 2023 information from the Epic Cosmos database that accounts for 26% of inpatient admissions within the U.S., Moin and colleagues assessed 3,453,687 grownup hospital admissions together with ICU care (n = 2,568,875; median age, 65 years; 55.3% males; 17.3% Black; 6.1% Hispanic/Latino) to uncover how in-hospital mortality, ICU size of keep and life-support intervention utilization have shifted during the last 10 years by evaluating outcomes from earlier than, throughout and after the COVID-19 pandemic.
“If you happen to needed to know [in-hospital mortality and ICU length of stay] and different associated measures after 2012 … you’d discover that there was a spot within the literature,” Moin mentioned.
“Epic Cosmos isn’t simply giant, it’s additionally actually consultant,” she added. “It contains sufferers from all 50 states and Washington, D.C., and it’s racially and ethnically various.”
In contrast with sufferers in 2014, Moin highlighted that sufferers in 2023 have been older (median, 66 years vs. 64 years), extra acutely in poor health primarily based on modified Simplified Acute Physiology Rating II (imply, 18.3 vs. 16.7) and had larger prevalences of a number of comorbidities together with persistent pulmonary illness, congestive coronary heart failure, persistent liver illness, malignancy, dementia and finish stage kidney illness.
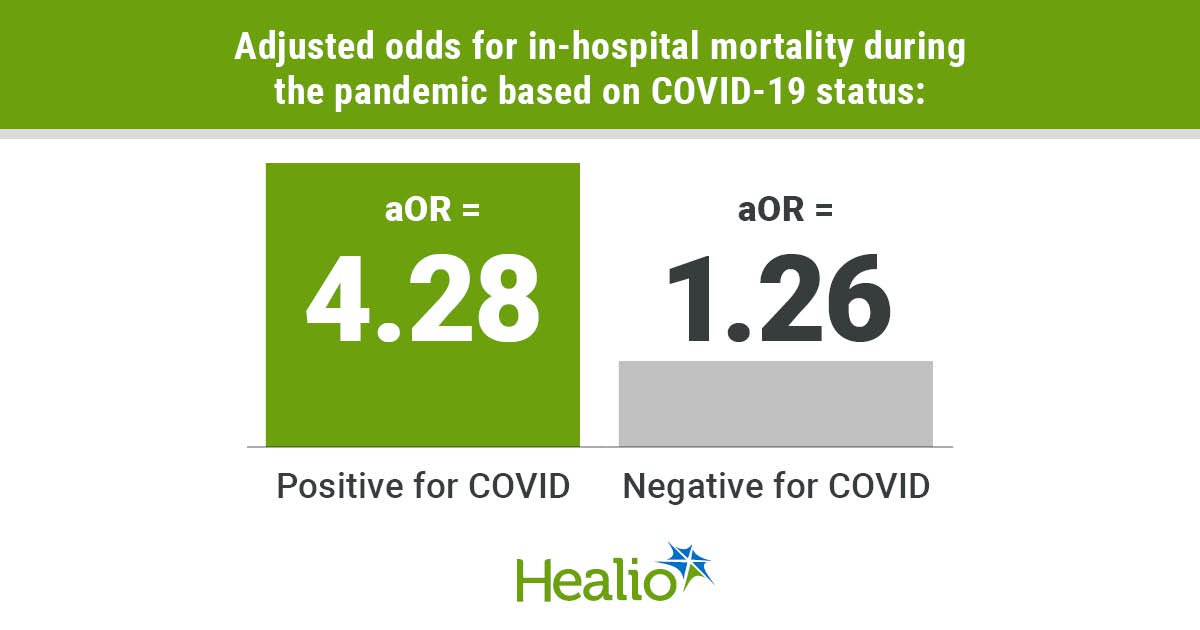
In a mannequin adjusted for affected person demographics, sickness severity and comorbidities, researchers discovered a better chance for in-hospital mortality throughout vs. earlier than the pandemic. Notably, elevated odds for this consequence have been present in each sufferers optimistic for COVID (adjusted OR = 4.28; 95% CI, 3.82-4.8) and sufferers detrimental for COVID (aOR = 1.26; 95% CI, 1.19-1.33). Within the years after the pandemic, particularly April 2022, Moin mentioned the chances for this consequence went again to the prepandemic baseline.
When it comes to ICU keep length, the median time went from 2.1 days earlier than the pandemic to 2.2 days in the course of the pandemic and remained at 2.2 days after the pandemic, in accordance with the examine. Researchers highlighted that this consequence differed in the course of the pandemic primarily based on COVID standing, with sufferers optimistic vs. detrimental for COVID having an extended keep (median, 4.1 days vs. 2.1 days).
The best fee of invasive mechanical air flow was noticed in the course of the pandemic (25.8%), whereas Moin famous decrease charges earlier than the pandemic (23.2%) and after the pandemic (22%).
“We noticed that ranges of invasive mechanical air flow declined, not simply again to their prior degree, however really additional down,” Moin mentioned.
“We’ll see within the coming years if that development continues, or if we degree out near the place we have been earlier than,” she added.
Moin additionally confirmed that vasopressor use was comparatively steady from 2014 (7.2%) by means of 2017; nevertheless, use started to rapidly rise throughout 2018 and was present in 21.6% of admissions in 2023.
“Beginning in 2018, we noticed a very fast enhance within the proportion of sufferers that obtained vasopressors, with really a tripling of that use from 2018 by means of the tip of our examine interval,” Moin mentioned. “That’s a change that properly precedes the onset of the COVID pandemic that we’ll want to seek out different explanations for.
“I feel {that a} actually thrilling avenue for future investigations will probably be understanding what drove that and what the consequences on our sufferers could have been consequently,” Moin added.
The examine additional reported that the proportion of stays with out vasopressors or invasive mechanical air flow noticed after the pandemic (66.7%) didn’t return to the proportion noticed earlier than the pandemic (72.5%) and was nearer to the proportion in the course of the pandemic (65.1%).