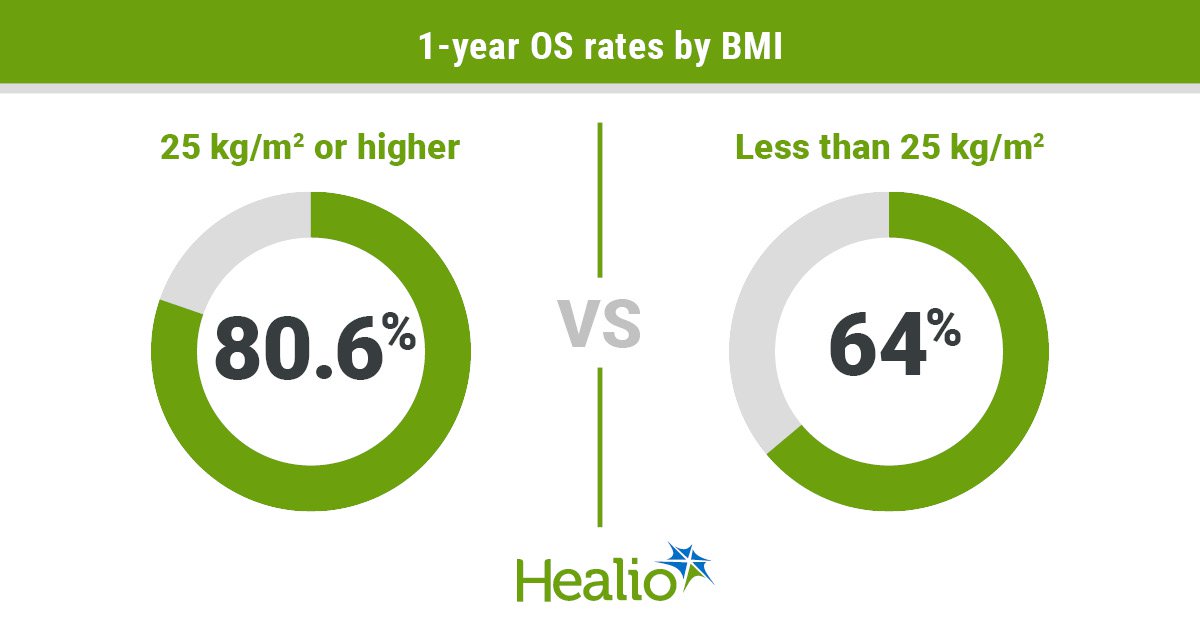
Key takeaways:
- An evaluation of two matched cohorts discovered improved 1-year survival amongst these with greater BMI.
- These with greater BMI additionally had decreased threat for ICU/hospital admission and several other different problems.
CHICAGO — An actual-world evaluation introduced at ASCO Annual Assembly supplied new insights into the impact BMI might have on how folks with most cancers reply to immunotherapy.
Sufferers with BMI of 25 kg/m2 or greater exhibited decreased 1-year mortality threat, in addition to a decrease threat for sure problems — together with ICU admission, pneumonia/pneumonitis or coronary heart failure — than these with BMI lower than 25 kg/m2.

Information derived from Albliwi M, et al. Summary 2603. Introduced at: ASCO Annual Assembly; Could 30-June 3, 2025; Chicago.
“These findings add to the proof that BMI is an important prognostic indicator of outcomes and problems after immunotherapy,” Moath Albliwi, MD, second-year medical resident at Cleveland Clinic Fairview Hospital, instructed Healio. “Danger stratification for any affected person who’s going to begin immunotherapy is necessary. We additionally want to ascertain some kind of calculator to assist us perceive how outcomes and problems might differ from one affected person to a different.”
Weight problems modifies cytokine profiles and alters immune cells, leading to adjustments to immune perform, in accordance with research background. A number of prior research demonstrated that individuals with greater BMI obtain higher response to immunotherapy, a discovering referred to as the “weight problems paradox.”
Albliwi and colleagues aimed to judge how BMI impacts immunotherapy outcomes — in addition to threat for main problems and hospital or ICU admission — amongst folks with strong tumors.
They used TriNetX, a platform that encompasses knowledge from 104 establishments world wide — to determine greater than 22,000 adults (age vary, 18-65 years) with one in every of 9 strong tumor malignancies: breast, head and neck, lung, kidney, endometrium, abdomen, esophagus and bladder most cancers, or melanoma.
All sufferers obtained at the least one dose of immunotherapy with a PD-1, PD-L1 or anti-CTLA-4 agent.
A majority of the cohort (61.7%) had BMI of 25 kg/m2 or greater, whereas 38.2% had BMI lower than 25 kg/m2.
Researchers used propensity rating matching to stability teams for intercourse, age, race, smoking standing, alcohol use and comorbidities, leaving 8,460 sufferers in every BMI group.
Outcomes included 1-year mortality, in addition to 1-year incidence of problems akin to ICU or hospital admissions, coronary heart failure, ischemic stroke/transient ischemic assault (TIA), myocardial infarction, venous thromboembolism, pneumonia/pneumonitis, polyneuropathy and acute kidney harm.
Outcomes confirmed a better 1-year OS price amongst these with BMI of 25 kg/m2 or greater vs. these with BMI lower than 25 kg/m2 (80.6% vs. 64%; P < .001).
This pattern endured throughout different BMI thresholds, as matched analyses confirmed improved 1-year OS amongst these with BMI of 35 kg/m2 or greater vs. these with BMI lower than 25 kg/m2 (83.2% vs. 64.6%: P < .001), in addition to amongst these with BMI of 40 kg/m2 or greater vs. these with BMI lower than 25 kg/m2 (82.4% vs. 63.8%; P < .001).
The group with BMI 25 kg/m2 or greater additionally exhibited decreased threat for sure problems. Researchers reported greater 1-year outcome-free possibilities on this group for ICU admission (89.1% vs. 83.3%; P < .001), hospital admission (48.1% vs. 37.5%; P < .001), ischemic stroke/TIA (95.9% vs. 94.6%; P = .001), pneumonia/pneumonitis (84.9% vs. 79.1%; P < .001) and coronary heart failure (87.6% vs. 84.3%; P < .001).
The findings recommend folks with low BMI might have a stronger inflammatory response to immunotherapy that ends in greater incidence of problems, Albliwi stated.
There is also proof within the literature that sufferers with greater BMI might have low-grade persistent irritation.
“Which may prime or stimulate the immune system in a greater approach to answer immune checkpoint inhibitors,” Albliwi stated.
Within the absence of a rating or calculator to enhance threat stratification, affected person training concerning the potential results of BMI on outcomes after immunotherapy can be necessary, Albliwi stated. Dose changes of immunotherapy based mostly on BMI additionally may very well be thought of, he stated.
“The subsequent necessary step is to grasp the variations in pharmacokinetic and pharmacodynamic exercise between these two teams of sufferers, and to conduct fundamental and translational analysis on the mobile degree to attempt to decide why folks with greater BMI have higher outcomes.”
For extra info:
Moath Albliwi, MD, may be reached at albliwm@ccf.org.