Key takeaways:
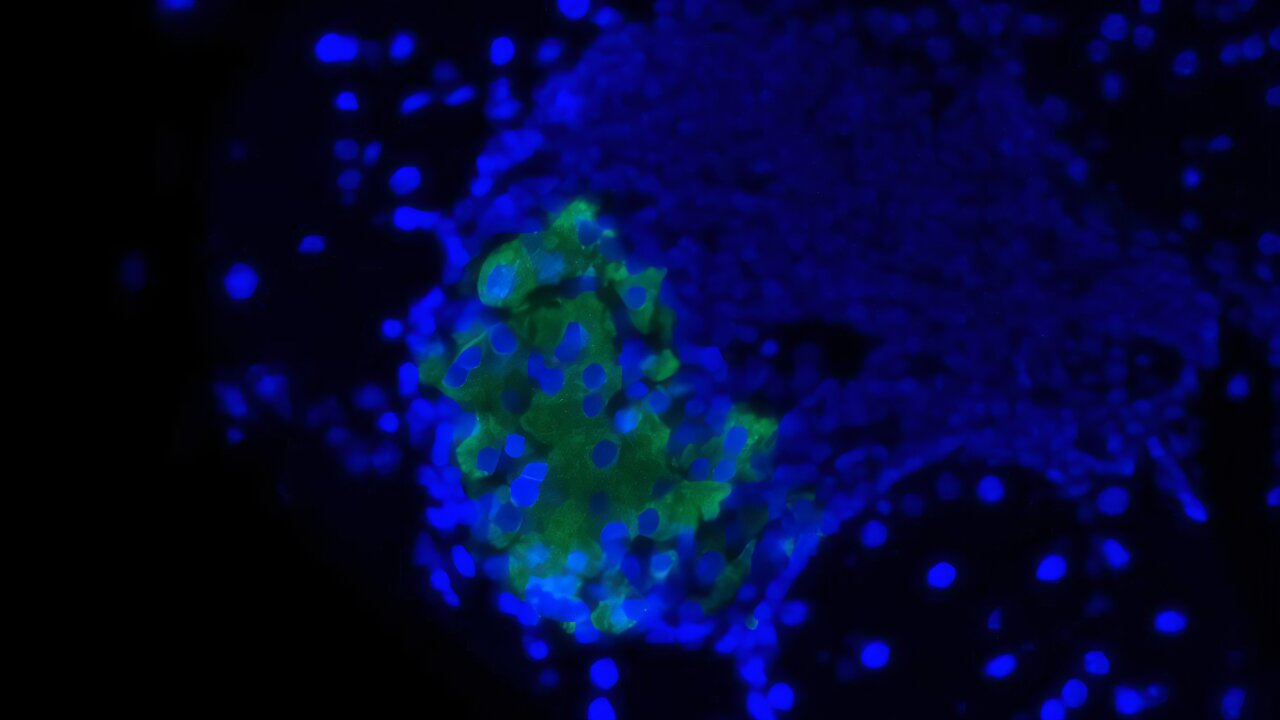
- Hyperpolarized xenon highlights air flow defects in MRI.
- Photographs have been taken earlier than and after bronchodilation at every go to.
- Adjustments in air flow defect percentages have been seen in responders at 4 weeks.
SAN FRANCISCO — Hyperpolarized xenon MRI could also be helpful in assessing response to biologic remedy amongst sufferers with bronchial asthma, in keeping with a poster offered on the American Thoracic Society Worldwide Convention.
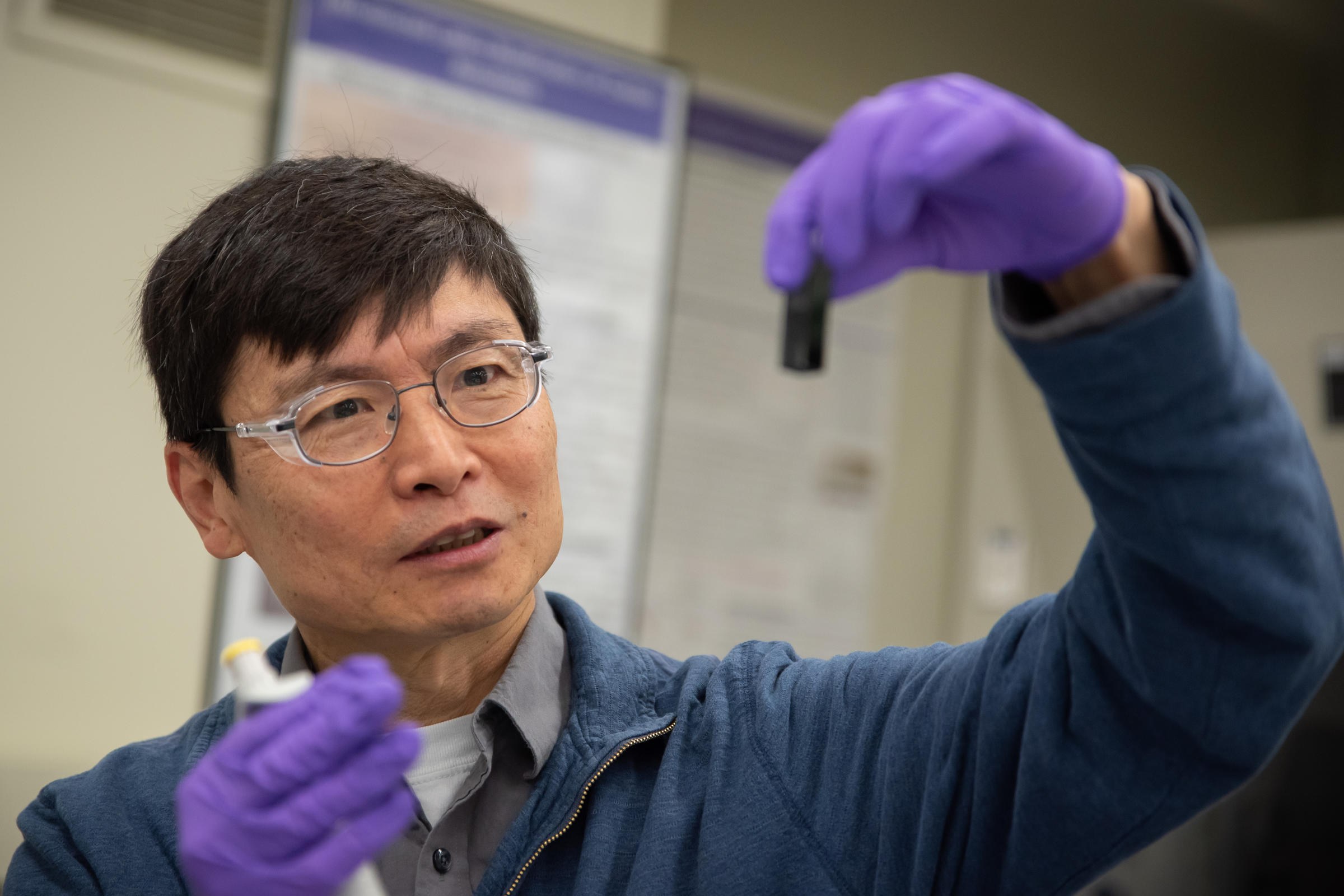
“Extreme asthmatics typically are handled with biologic remedies,” Gabriela María García Delgado, analysis pupil, chemical and biomedical engineering, College of Missouri, informed Healio. “A few of them do reply nicely.”

Information have been derived from Garcia Delgado GM, et al. Using hyperpolarized 129Xe MRI as a biomarker for asthmatics on biologic remedies. Introduced at: American Thoracic Society Worldwide Convention; Might 16-21, 2025; San Francisco.
However sufferers who don’t reply nicely have to search for options, she continued, resulting in continued poor high quality of life, increased prices and misplaced time as these choices are examined.
“Our purpose was to make the most of hyperpolarized gasoline MRI in a longitudinal examine and quantify their air flow defect share and their cluster index,” García Delgado mentioned. “That manner, we will truly see and quantitatively assess their adjustments.”
Findings could recommend that sufferers usually are not responding to remedy, she mentioned.
“In the event that they’re not feeling like they’re bettering at this level, is it time to alter to a different biologic or a mix of medicines?” García Delgado mentioned.
The examine comprised 5 responders and 7 nonresponders to biologic remedy for extreme bronchial asthma, together with mepolizumab (Nucala, GSK), benralizumab (Fasenra, AstraZeneca) and dupilumab (Dupixent; Regeneron, Sanofi).
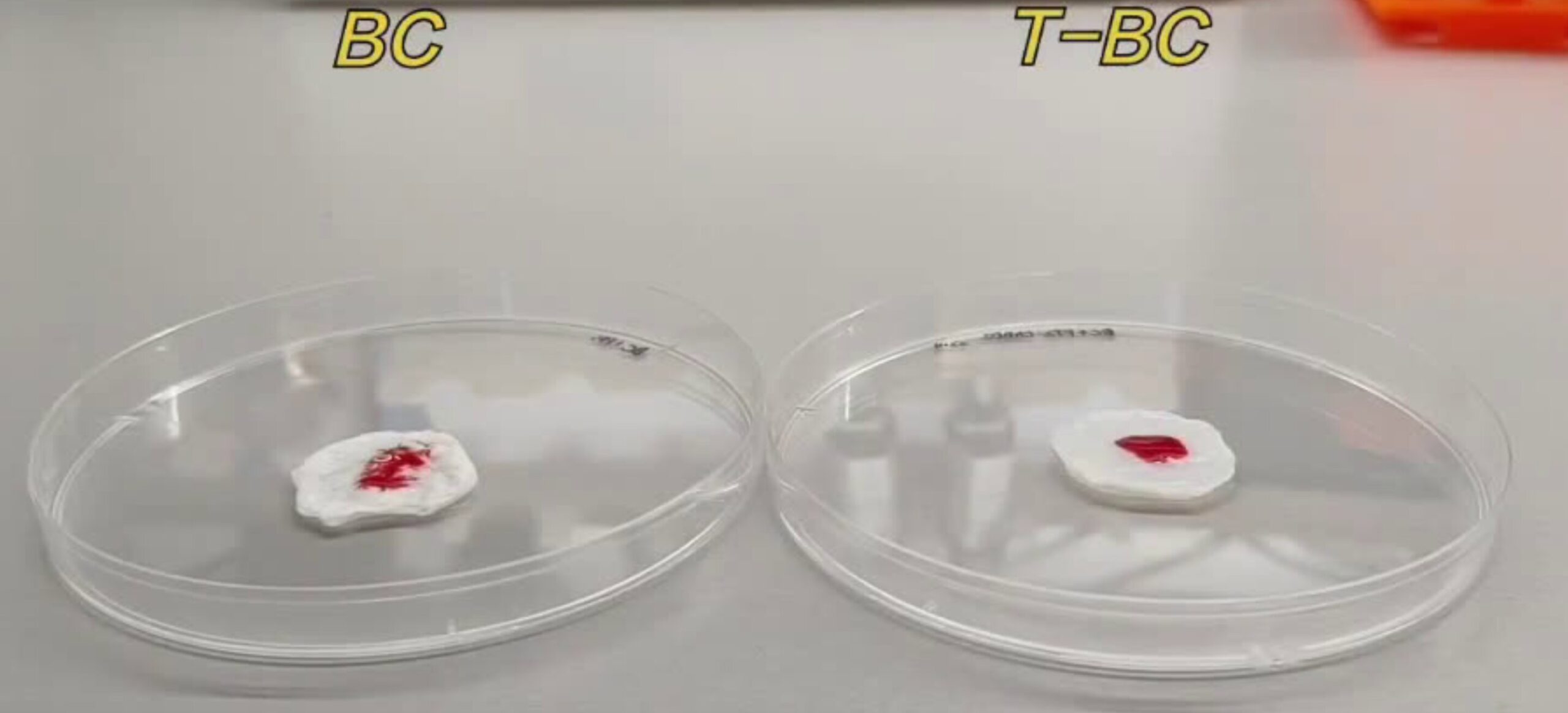
Sufferers had a hyperpolarized xenon MRI, bloodwork, questionnaires and pulmonary operate testing (PFT) at baseline and at 4 and 12 weeks after initiating remedy. Imaging was administered earlier than and after bronchodilation at every go to.
“The sufferers are within the scanner. We give them the hyperpolarized gasoline,” García Delgado mentioned. “Then they do a small breath maintain, often 16 seconds, and we purchase the imaging. At that time, then we do all of the post-processing evaluation.”
The researchers labeled sufferers as responders or nonresponders at 12 weeks.
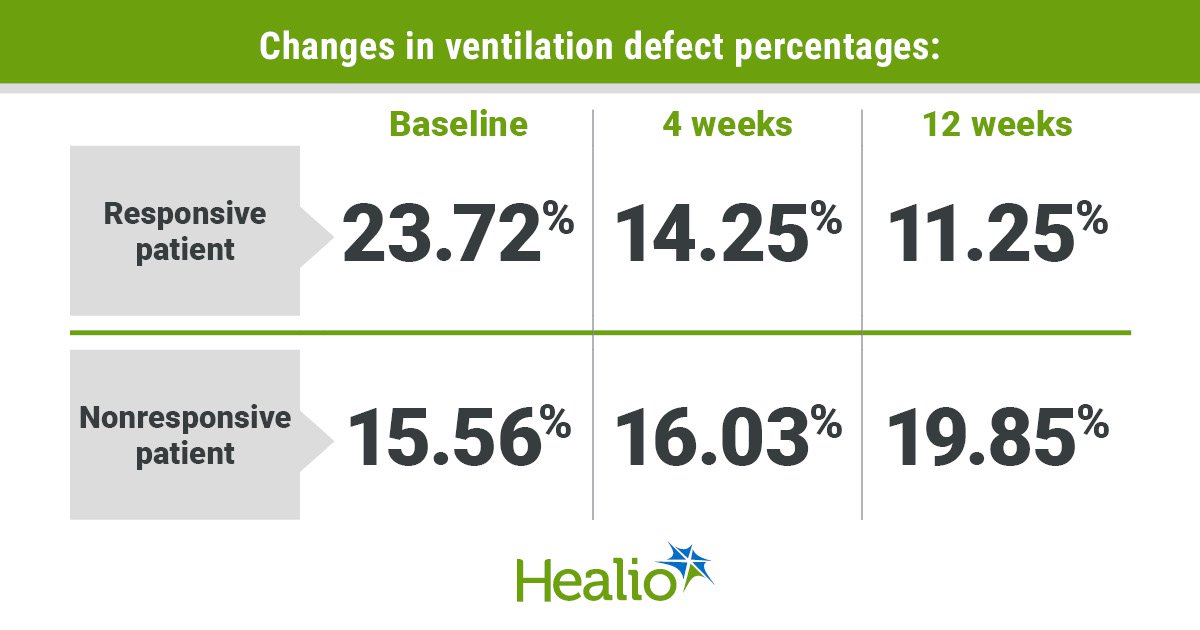
One responsive affected person, a person aged 70 years, had a air flow defect share (VDP) of 23.72%, a cluster index (CI) of 28% and a FEV1 p.c predicted of 95.9% at baseline.
By week 4, VDP fell to 14.25%, CI fell to 16% and FEV1 p.c predicted elevated to 105.3%. At week 12, VDP was 11.25%, CI was 19% and FEV1 p.c predicted was 95.9.
“Their defects are literally going away,” García Delgado mentioned. “It means they’re ventilating higher.”
One nonresponsive affected person, a girl aged 72 years, had a 15.56% VDP, 18% CI and 65.5% FEV1 p.c predicted at baseline. At week 4, VDP was 16.03%, CI was 18%, and FEV1 p.c predicted was 58.1%. Equally, VDP was 19.85%, CI was 23% and FEV1 p.c predicted was 56.6% at week 12.
“Once we have a look at her photographs, we will additionally see that they actually didn’t reply a lot,” García Delgado mentioned.
Visible evaluation indicated a downward development within the VDP boxplots of the responders and an upward development within the VDP boxplots of the nonresponders, though García Delgado mentioned this development was not vital.
Nevertheless, the rise in imply pre-bronchodilation VDP from 11.6% at baseline to 12.2% at 12 weeks was vital (P = .03), she mentioned. The change in imply CI from 4 weeks (15.3%) to 12 weeks (16.9%) was vital as nicely (P = .03), she added.
“We’re making an attempt to evaluate how they enhance, the place they enhance and, particularly in the event that they’re bettering, how quickly can we detect that enchancment,” García Delgado mentioned. “We would like to have the ability to present extra of a personalised strategy to drugs.”
Primarily based on these findings, García Delgado mentioned that FEV1 p.c predicted does probably not present that info as a result of it’s extra of a worldwide measure.
“Hyperpolarized gasoline, VDP and CI — particularly CI — is extra of a regional and extra focal evaluation of their enchancment,” she mentioned.
García Delgado additionally famous that PFTs rely on affected person cooperation, with some sufferers unable to even carry out the testing. She additionally mentioned that she and her colleagues didn’t see many variations in fractional exhaled nitric oxide testing between the teams.
Additional, García Delgado mentioned the subjective nature of the Bronchial asthma Management Questionnaire could make response tough to quantify.
“It simply depends upon how they’re feeling,” she mentioned. “Hyperpolarized gasoline could present info that questionnaires and PFTs possibly received’t.”
The researchers are recruiting extra sufferers with extreme bronchial asthma for the continued examine.
For extra info:
Gabriela María García Delgado may be reached at gmg9r2@missouri.edu.